Is technology the cure for the loneliness epidemic?
February 9, 2024Age Tech,Senior CareBlog
Senior-aged adults experienced a loneliness surge during the height of the Covid-19 pandemic. Yet, even before the pandemic, 40% of adults over age 65 reported feeling lonely. This makes sense when we consider that social isolation is a major cause of loneliness in senior-aged adults. Despite fewer Covid-19 hospitalizations, the Covid-induced increase in social isolation continues to persist among senior-aged adults. Technology use was embraced by many seniors during the pandemic mainly due to its capacity to enable online interpersonal connections. Medical research findings published in 2022 confirmed this increased Internet and digital device utilization among the elderly due to the Covid-19 pandemic.
The causes of senior-aged social isolation
Nearly four in 10 senior-aged adults live with extended family worldwide. However, those in the US rarely do. As of 2020, 28% of community-dwelling seniors lived alone. While death of a spouse or dementia in a spouse are major reasons for increased social isolation among older-aged adults, an increased amount of disability and death among longstanding friends is another cause. The following are four other causal factors:
- Relocation by adult children to a new residence far from their senior-aged parents;
- Worsened eyesight, leading to reduced driving to engage in social interactions;
- Chronic health disorders and physical disabilities that limit visiting family and friends;
- Higher risk to contract an infection resulting from large social gatherings.
At least 50% of adults aged 60 or older are at risk for social isolation, with 33% expected to experience a high degree of loneliness in future, per a recent article in BMC Public Health. In turn, this reveals that a loneliness epidemic in senior-aged adults requires immediate attention.
The link between loneliness, depression, and chronic health disorders
Loneliness can lead to chronic depression in both younger and older adults. However, chronic depression in seniors is also strongly-linked to the development of the following chronic health disorders:
- High blood pressure;
- Heart disorders such as arrhythmia;
- Obesity;
- Alzheimer’s disease and other dementias
According to the National Institute of Mental Health, chronic depression also increases the risk for chronic pain. In addition, it increases the risk for sleep disorders such as insomnia. Notably, sleep disorders are linked to an increased risk for depression and numerous chronic health conditions. Most of all, chronic depression and sleep disorders both tend to lessen the brain’s release of certain biochemicals – such as Serotonin – that boost mood and stave off depression.
Mental health benefits of technology utilization in the elderly
At 70 years of age, two out of three adults in the US have some level of cognitive impairment, most commonly short-term memory deficits and worsened reflexes. Overall, mental health is worsened by cognitive impairments (such as decreased problem-solving capacity). Since chronic depression as well as diverse chronic health disorders can foster increased cognitive impairments, engaging in digital “brain health” activities in can be beneficial for preserving cognitive functioning.
Brain plasticity & technology use
Brain plasticity—meaning the capacity for creating new nerve pathways in the brain—boosts cognitive ability and overall brain health. While younger brains have a higher degree of brain plasticity, findings published in Frontiers in Aging Neuroscience have shown that the elderly can also boost their brain plasticity. This is a particular reason that learning new information and skills (such as the use of tech gadgets) is especially beneficial for the mental health of senior-aged adults.
Additionally, continuous learning activities have been clinically recognized as protective of cognitive functioning in senior-aged adults. Therefore, learning new technology programs and digital devices can aid elderly individuals to both preserve their level of cognitive function, as well as interrupt further cognitive decline.
How technology can address the loneliness epidemic
While technology by itself cannot “cure” the loneliness epidemic, it can certainly help. Senior quality-of-life can be improved by interacting with others via technological approaches, which can boost both mental/emotional well-being and overall health.
Videoconferencing programs and social media have enabled interpersonal communication to continue among adults living with disabilities that limit their capacity to attend “in-person” social activities. This is especially the case for disabled senior-aged people who can no longer venture far from home. In this way, technology utilization can both lessen social isolation and loneliness – thereby reducing the likelihood of worsened mental health and physical health.
Ōmcare not only serves as a medication reminder and telehealth interface, but it also connects seniors to loved ones with the simple touch of a button. To learn more about how we’re bringing health and connection into the home, visit omcare.com.
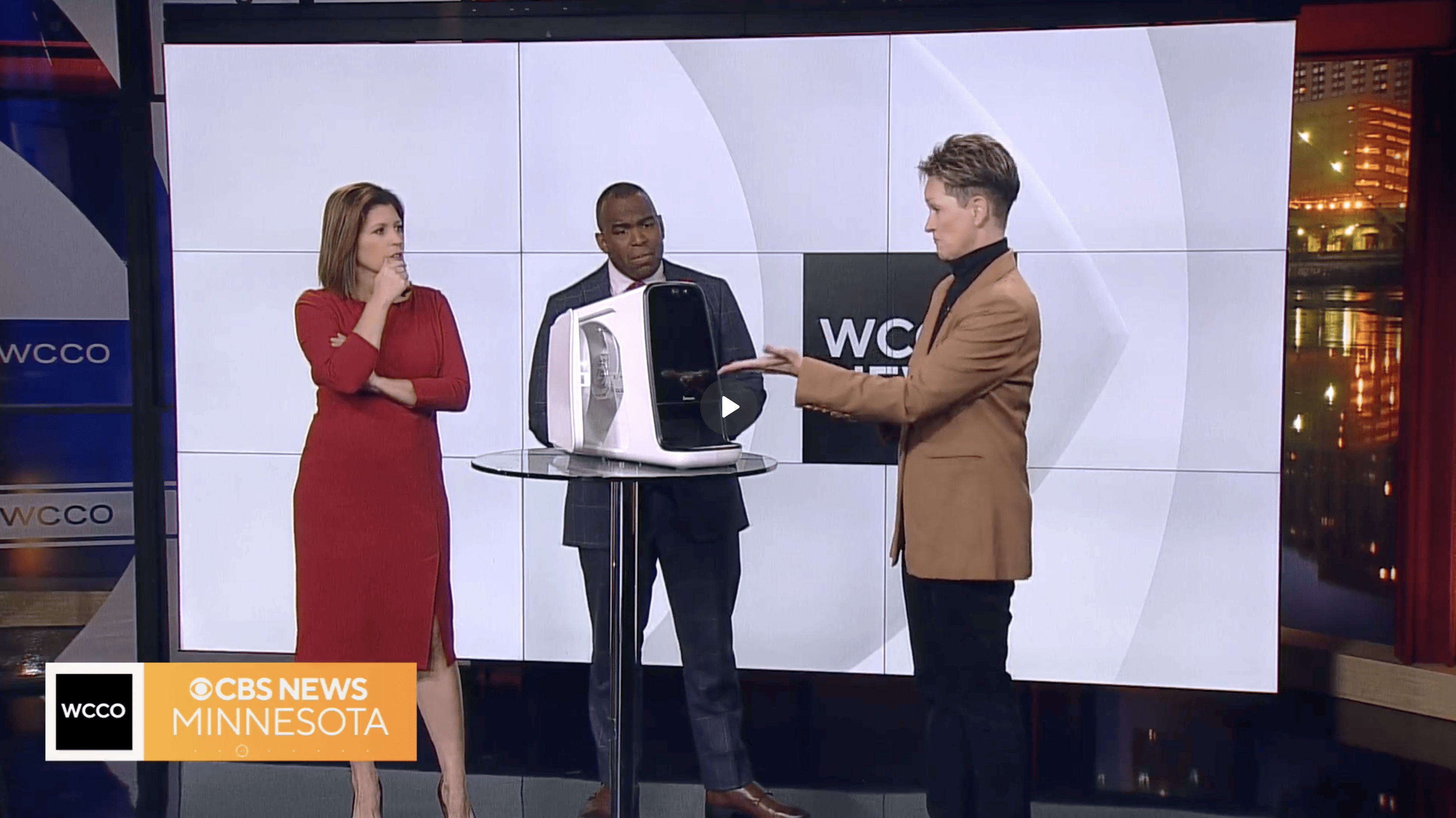
Ōmcare talks about the importance of monitoring your health with CBS News Minnesota, 1/29/24
National Self-Check Month stresses importance of regular health checks. Watch Morgan Rogers from Ōmcare talk about the importance of monitoring your health.
Watch the full news clip from CBS News Minnesota here.
Ōmcare recognizes National Family Caregivers Month with CBS News Minnesota, 11/21/23
"Bloomington based Ōmcare wants to make the job of caregiver as easy as possible. CEO Lisa Lavin talks about how they're doing that."
Watch the full news clip from CBS News Minnesota here.
WDIO Feature: New telehealth solution called Ōmcare Home Health Hub is aimed at helping people live independently for longer
A beautiful apartment overlooking Lake Superior is a treasured place for many at Ecumen Lakeshore in Duluth.
People want to live independently longer. But one thing that can get in the way is the complication of taking multiple medications.
Lisa Lavin, founder of Ōmcare, was inspired to do this after watching her beloved grandmother fade away in a way that didn’t allow her the respect that she deserved.
So after years of research and development, including starting with a device that dispensed pet treats, they’ve launched the Ōmcare Home Health Hub.
Lavin explained, “We’ve directly connected with the pharmacy data system. They will fill your meds in a pouch format, which is delivered to your home. And then it’s put in your health hub. You can use the smart assistance, which is digital reminders for you. Or caregiver assistance, which is when someone will call you through the hub to remind you to take the meds.”
Watch the full news clip from WDIO here.
Ōmcare Collaborates with Leading Senior Care Providers to Change Care Models for the Aging Population
October 24, 2023PressPress Releases,News
- Ōmcare is launching an all-in-one technology platform to extend the reach of caregivers into the home and enable remote medication assistance that promises dose-level medication adherence.
- Ōmcare is collaborating with senior care providers, like Minnesota-based Ecumen and Ohio-based Continental Senior Communities, to accelerate their home care strategy. The new solution is entering the market at a critical juncture for the healthcare industry as more aging Americans are living longer with increasing chronic conditions and wanting to age in place at home, but doing so at a time when access to caregivers is falling.
- Ōmcare has integrated directly with national pharmacy information systems, allowing for seamless home delivery of medication for dispense and visual confirmation of adherence by the Ōmcare Home Health Hub®. This bridges a critical gap in the healthcare sector's ability to ensure the right medication, at the right time, for the right person.
[Minneapolis, October 24, 2023]. Today, Ōmcare announced that it is launching the Ōmcare Home Health Hub®, an all-in-one, customizable home health platform that allows care providers to extend care into the home via a secure infrastructure with one-touch access to telehealth services, aggregated remote patient monitoring, and medication dispensing with visual confirmation of dose-level medication adherence.
"Ōmcare exists due to the rapidly aging population; high rate of medication nonadherence; a shortage of family and professional caregivers; continued increase in health care costs; the need for in-home care and aging in place;" remarked Lisa Lavin, the CEO of Ōmcare. "Ōmcare opens up the home as a legitimate site of care by creating an all-in-one, easy-to-use solution with a comprehensive suite of capabilities required for remote care."
Ōmcare allows health care and senior care organizations to rapidly deploy a home care strategy while simultaneously customizing the provider and patient experience to fit their brand. The product's accessible architecture also allows for the integration of provider and consumer tools aimed at:
- Addressing the increasingly complex care needs of the Over 65 and dual populations.
- Delivering a platform that allows for tailored customization of current chronic and acute solutions.
- Extending caregiver reach and efficiency.
- Promising right medication, right time, right person.
To support a seamless consumer experience, Ōmcare integrates directly with pharmacy information systems enabling Ōmcare Home Health Hub users to know their medication schedule and receive timely alerts and medication assistance events. This integration delivers a comprehensive last-mile solution to address medication non-adherence, a problem that costs the healthcare industry more than $500 billion a year. More than 33% of hospital readmissions result from medication non-adherence as do 150,000 deaths each year. The novel relationship between Ōmcare, pharmacy and senior care providers is the first of its kind that will increase patient access to the care they need and empower clinicians with better visibility into whether or not patients are adhering to the medications they have been prescribed.
Medication adherence among older adults with chronic conditions taking multiple medications can be hindered by forgetfulness, the complexity of regimens, functional status, and other factors. Non-adherence is a leading driver of hospitalization and loss of independence. For senior care providers like Ecumen and Continental Senior Communities—the Ōmcare Home Health Hub serves as a portal for new services that help people maintain independence in their homes longer.
"Medication administration is one of the care needs that cause people to move into higher levels of care. Keeping residents in the lowest level of care and the highest degree of independence is critical for improved lifestyle, longevity and cost-effectiveness," said Eleanor Alvarez, Board Chair of Continental Senior Communities and CEO of LeaderStat. "The Ōmcare Home Health Hub's ability to provide remote care and ensure medication adherence sets a new bar in the industry and aligns with our innovation mindset."
"People are most comfortable when they are living where they want to live. Ecumen is dedicated to creating a home for older adults, wherever they choose to live," said Brett Anderson, Chief Ecosystem and Operating Officer of Ecumen. "We help them do that through innovations like the Ōmcare Home Health Hub, which helps residents maintain greater independence longer."
The Ōmcare Home Health Hub offering is available now through select senior care providers to bring telehealth services into the home to improve outcomes, reduce cost, increase member engagement, and elevate patient experience. For updates on the Ōmcare Home Health Hub, visit www.omcare.com.
About Ōmcare
Ōmcare is a digital health company pioneering a customizable, all-in-one home health platform that allows healthcare organizations to extend care into the home via a secure telehealth infrastructure with one-touch access to telehealth services, aggregated remote patient monitoring and medication dispensing with visual confirmation of dose-level medication adherence. Ōmcare is an AARP Innovation Labs portfolio company. It was recognized as one of the "top innovations" by the New York Observer and has been heralded by the Accenture HealthTech Innovation Challenge as one of the most innovative startups serving North America focused on solutions for health organizations. To learn more, visit www.Omcare.com/contact-us-providers/.
Media Contact: Megan Rogers
612-351-3780
meganr@media-minefield.com
www.omcare.com
Why medication adherence is important and how to improve it
July 17, 2023Age Tech,Senior CareBlog
Most adults with chronic health disorders are treated with medication, vitamins and minerals, or hormones. However, 50% of adults in the US living with chronic disorders do not take their daily medication (or other self-administered oral or IV therapies) as prescribed. According to a research article in The Permanente Journal, this results each year in around 100,000 preventable deaths and $100 B in preventable healthcare costs. Forgetfulness is not the only reason that medication nonadherence is so widespread, but this is a particular problem for the homebound elderly. Besides leading to worsened health status, not taking medication as prescribed is contributing to a worldwide public health problem.
Impact of antibiotic nonadherence and drug-resistant infections
The diagnosis of a skin, urinary tract, respiratory, or other bacterial infection often requires treatment with an oral antibiotic for five to seven days to eliminate the infection. However, people typically begin to feel better earlier than the last prescribed dosage day, so discontinue taking the prescribed antibiotic pills. Consequently, the bacteria that cause human diseases are becoming more drug-resistant. The Centers for Disease Control (CDC) reports that 2.8 million drug-resistant infections occur in the US per year, and with an estimated 35,000 resultant deaths. Therefore, the common occurrence of patients not taking a prescribed antibiotic for the full course prescribed to them has led to more bacteria becoming resistant to all antibiotics.
Methicillin is an antibiotic that is a derivative of penicillin, and people afflicted with Methicillin-Resistant Staph. Aureus (MRSA) infections are 64% more likely to die from this type of antibiotic-resistant infection. Since Staph. aureus is one of the most common skin infection-causing bacteria (as it is commonly found on our skin), the increasing ability of this bacteria to survive all antibiotic treatments is causing tremendous medical concern. Meanwhile, surgical patients remain the ones at highest risk for developing a Staph. aureus infection in the incision site, but MRSA can also be transmitted by an infected person to someone else through hand-to-skin contact. In 2019, 27,314 MRSA-infected people in high-income countries alone (and 93,767 elsewhere) died due to their antibiotic resistance.
Nonadherence to blood pressure medication and consequences
Nearly 66% of people diagnosed with hypertension who are prescribed drugs to lower their blood pressure are nonadherent to medication treatment, per an article in Medicine in 2017. Since 70% of adults aged 65+ have hypertension – and hypertension is strongly linked to a heightened risk for heart attack and stroke – lessening the prevalence of hypertension (high blood pressure) has been a major US healthcare goal to curb national healthcare costs. Meanwhile, heart disease is the foremost chronic health disorder in the US, and the leading worldwide cause of death in adults.
Diabetes Type-2 and nonadherence to medication
Study findings published in Patient Preference and Adherence revealed that 45% of adults with diabetes (Type-2) are not able to maintain glucose control, and poor medication adherence is a major reason. The lack of taking medication aimed at glucose control can result in diabetes-afflicted people developing diabetes complication such as peripheral neuropathy (nerve pain), heart disease, and kidney failure. In turn, these complications can result in permanent disability and a far lower overall “quality-of-life”.
Reasons for medication nonadherence
Described in a medical research article in 2019 are the following five dimensions that affect patient adherence to their prescribed medication:
- Social and economic factors (such as ability to afford the prescribed drugs);
- Therapy-related factors (such as understanding why the drugs are necessary);
- Disease-related factors;
- Patient-related factors;
- Healthcare system-related factors
For adults aged 65+ who are enrolled in a Medicare Part D drug plan, there are wide variations in the cost of a prescribed medication that must be borne by the enrollee. If not enrolled in a Part D drug plan (or without any other drug coverage), the older-aged person may be faced with paying for the medication “out-of-pocket”.
The average annual cost of taking an oral glucose-lowering medication to manage diabetes (Type-2) in 2017 was $2,727 – which had increased by 147% from 2015. It is well-recognized that the cost of prescribed medication to control diabetes (Type-2) is high, and this is a main reason that diabetics do not take the prescribed medication that could preserve their health and prevent premature death. Therefore, seniors – many of whom are living on fixed incomes – often fail to take their prescribed medication.
A tremendous problem for elderly people is polypharmacy – which is the daily taking of many prescribed drugs aimed at different health disorders. For example, a senior living with diabetes (Type2) may also need to take medication for heart disease, nerve pain, a scrape on the foot that has become infected, low thyroid level, and many other health problems. Consequently, mixing up pills (and taking too many of one drug and not enough of another) can easily occur.
Cognition worsens during aging – even in elderly adults not living with Alzheimer’s Disease – so remembering whether a given pill was taken or not with breakfast every day can become difficult. This type of forgetfulness can leave any older-aged person who has been prescribed multiple medication feeling extremely frustrated. Furthermore, the Alzheimer’s Association notes that around one in nine adults aged 65+ has Alzheimer’s Disease, so forgetting to take prescribed medication (and/or mixing them up) is even more likely in these senior-aged adults.
Strategies that foster improved medication adherence
Physician office phone calls to remind older-aged people to take their prescribed medication have been found to be effective in promoting medication adherence, as have daily text messages and automated reminders on digital wearables. Meanwhile, calls from pharmacies – and especially if an existing medication prescription is not re-filled – have been found to be effective, as well.
Besides reminders, physician-initiated discussions about the financial impact on a patient of a prescription can enable recognition if cost is the main factor. In that case, helping the patient to learn about ways to reduce the cost (such as through enrollment in a clinical trial where drug cost may be covered) can boost adherence to prescribed treatment.
Learning that a different Medicare Part D plan covers the cost of a specific prescribed drug (and then switching plans during Medicare’s “open enrollment” period) may be all it takes for a person with a history of medication nonadherence to change that behavior. The ease of comparing health insurance plans is increased for seniors through access to computer training in combination with ownership of a computer, so independent and assisted living facilities geared to older-aged adults can be part of the solution by engaging their residents in utilizing technological devices.
The Ōmcare Home Health Hub is an all-in-one home telehealth device aimed at senior-aged adults, and that can be used to promote medication adherence.
Senior care facilities: How to encourage age-tech adoption
June 26, 2023Age Tech,Senior CareBlog
Learning new skills helps seniors to maintain cognitive abilities such as problem-solving. Since most adults aged 65+ did not grow up utilizing technology, it is not something that many senior-aged people feel is necessary for them. Nevertheless, the gap in digital device use between the 18-29 year old age demographic and adults aged 65+ has closed by 53 percentage points since 2012, per the Pew Research Center. At least six in 10 adults aged 65+ now utilize the Internet to acquire some type of information. Assisted living facilities, rehab centers, and nursing homes can aid senior-aged people to preserve mental faculties and reduce symptoms of depression and/or anxiety by improving senior-oriented tech device understanding.
Why senior-aged adults have difficulty learning to utilize technology
The language of technology is unfamiliar to many older-aged adults, so tech support instructions that make sense to a younger adult can sound like gibberish to an elderly person. Even telling a senior-aged person to click on an “icon” on the computer screen can make utterly no sense, as this is not the definition of that word in the dictionary of their childhoods. Therefore, online instructions to aid technology learning can be totally ineffective. Instead, a person teaching hardware and/or software skills on a one-to-one (or small group) basis works best for older-aged adults.
Providing “in-person” training and classes is just one way to boost interest in age-tech adoption, as family members and senior care facility employees may also be able to teach the older-aged person some desired tech skills. By increasing the size of fonts (so that the senior using the tech device can more easily see what is on the screen) and enabling voice-activation, the common problems of decreased eyesight and arthritic fingers to manipulate a tech device can be greatly minimized.
Findings published in Frontiers in Psychology in 2017 revealed that lack of guidance plus lack of confidence and/or feelings of inadequacy were key reasons for seniors’ disinterest in using digital devices.
Enabling seniors to utilize videoconferencing for clinician visits
Socialization and communication with others are a strong motivator for elderly people to learn to utilize videoconferencing software on digital devices. However, another motivator is reducing the need for travel to an office appointment with a physician (or other clinician) through the utilization of videoconferencing software on a digital device to participate in a “telehealth” visit. According to Fierce Healthcare, telehealth utilization has increased by 340% among Medicare-eligible senior-aged adults since the onset of the Covid-19 pandemic. One major reason is that it decreased the likelihood of contracting Covid-19 (or some other respiratory infection) in the physician’s office or hospital setting.
For a senior care facility to appear attractive to a person aged 65+ in comparison to some other facility, demonstrating a willingness to aid seniors in acquiring and learning technological devices can be an important factor. Loss of former mobility and/or symptoms of dementia are major reasons that elderly people (and their family members) choose to relocate to assisted living facilities and other senior care facilities. Consequently, senior care facilities that offer computer rooms, tech-related classes, and the ability to engage in a telehealth visit with an on-site clinician are more appealing to elderly people than ever before.
The Population Research Bureau estimates that nine million senior-aged adults in the US will be living with dementia by 2030, and 12 million by 2040. Many of them will require placement in a senior care facility, so embracing the utilization of technology by seniors can aid them in remaining as functional in their usual daily living activities as possible.
Ōmcare provides technology solutions for both consumers and providers, and inclusive of senior care facilities.
Employee Spotlight: Abiola Adimi
June 8, 2023Employee SpotlightBlog
Name: Abiola Adimi
Title: Senior Software Engineer
Education: Bachelor of Science in Computer Engineering from University of Minnesota Twin Cities
Time at Ōmcare: 5 years
One personal fact about you: Big Fan of Japanese Anime (Favorite: One piece has been running for 20+ years)
1. What led you to Ōmcare?
I joined Ōmcare in July 2018 as an intern because of how impressive the original product PetChatz was and how welcoming the engineering team was — they had no prejudice and were willing to help where I was lacking.
2. What’s the most rewarding part of working at Ōmcare?
The most rewarding thing about working at Ōmcare is the opportunity to be part of a dynamic and innovative team that consistently strives for excellence. Ōmcare fosters a culture of collaboration and encourages employees to bring their ideas to the table. This open and inclusive environment empowers me to contribute my unique skills and perspectives, knowing that my input is valued and appreciated.
3. What is your favorite current project you’re working on?
I’m currently working on testing the software infrastructure on the new hardware that will be used for our next generation project Hub 2.0. Using an iMX 8 devkit, I have begun the preliminary work to port our existing software and test new features.
4. Pick out a core value that means a lot to you. How have you seen this lived out in your time at Ōmcare?
We boldly go where no one has gone before: This value is one of the reasons I wake up to work every morning with a new goal to achieve. Since my internship days, I have always been encouraged to think beyond conventional solutions and traditional approaches. With a culture that promotes curiosity, creativity, and entrepreneurial opportunities, I am never bored or uninterested in my work. Every new challenge is an opportunity for me to grow in different aspects. By stepping out of our comfort zone into unknown territories, we have always achieved extraordinary outcomes to deliver an excellent product to our customers.
5. What are you most proud of accomplishing throughout your time at Ōmcare?
Having been part of the development of our current Hardware/Software development infrastructure, my proudest accomplishment while at Ōmcare would be my growth as an experience and almost all-rounded Computer Engineer, who is not afraid of new challenges. Computer Engineers deal with a lot of unknowns while dealing with the hardware and software aspects of a product. During my time at Ōmcare, my analytical and creative skills are always being sharpened to implement new features that our customers will be able to experience seamlessly and with a smile on their faces.
6. Why should someone work at Ōmcare?
Work plays a vital role in our lives, providing us with numerous benefits and opportunities for personal growth. Ōmcare is a company that offers a lot of opportunities for growth. To grow, people need challenges and a sense of adventure. Thus, I believe that as a startup company where everything is fast paced and riddled with unknowns, people should work at Ōmcare if they believe that they are in a stage of their lives where they would like to make a difference in the healthcare world without any fear of challenges.
Managing the rising costs of healthcare: Your Medicare options
June 5, 2023Medicare AdvantageBlog
Medicare coverage is aimed at adults aged 65 and older, as well as younger disabled adults. While some senior-aged people are not insured by Medicare, it has enabled most adults aged 65+ in the US to acquire health insurance coverage. There are four distinct parts to this federal health insurance program administered by the Centers for Medicare and Medicaid Services (CMS), and these are Parts A, B, C, and D. Unlike Parts A and B, Medicare Advantage health insurance (Part C) is administered by private health insurance companies through CMS subcontracts. Meanwhile, Part D covers prescription medications (and is also offered by private insurers). For this reason, enrolling or switching coverage options can be extremely confusing for most adults.
Enrolling in Part A versus Part B
Original Medicare’s Part A covers primarily hospitalization, whereas Part B covers outpatient healthcare visits. At three months prior to becoming 65 years of age, a senior can enroll in Original Medicare (and coverage then becomes effective at age 65). Part A enrollment does not result in a monthly premium cost for most seniors, so it makes sense to enroll unless covered by some other health insurance. While Part B does have a premium cost linked to it, coverage via this part can make a huge financial difference since most seniors need outpatient medical care even more than younger adults. Since Parts A and B do not cover all healthcare costs, it is important to plan for future medical bills upon needing either inpatient or outpatient services. For example, both Parts A and B have annual deductibles that must be met before Medicare covers the rest of the billed dollar amount.
Understanding Part A costs for the hospitalized enrollee
The deductible for Part A is $1,600 per benefit period in 2023. Besides factoring in this cost as something that is the enrollee’s financial responsibility, it is crucial to realize that the enrollee’s cost is $0 through Day 60 of the hospitalization, but increases to $400 per day for Days 61-90 (with a maximum out-of-pocket cost that may be changed annually by the CMS). The average (mean) hospital stay in the US is 4.7 days, with a mean total cost of $11,700 per day. Thus, a lack of health insurance can quickly lead to a tremendous debt-load for an adult in the US.
Part B co-insurance and deductible costs
Part B costs more for enrollees above a specified annual income threshold. However, $164.90 was noted by the Medicare.gov website as the typical monthly deductible cost for 2023. Furthermore, Part B covers only around 80% of the billed amount for each outpatient visit or service, so 20% of the cost is the responsibility of the Medicare-enrolled senior. On the other hand, Part B does not require the enrollee to have a Primary Care Physician (PCP) and allows the enrollee to receive Medicare-covered care from any doctor that accepts Medicare.
Original Medicare versus Medicare Advantage
The Kaiser Family Foundation (KFF) in 2022 reported that enrollment in Medicare Advantage has continued to grow over the past 20 years, and around 48% of Medicare beneficiaries are now enrolled in a Medicare Advantage plan. Although most Medicare Advantage plans include prescription drug coverage, they also usually limit the choice of physicians and hospitals to those that are “in-network” (plus include selecting an “in-network” PCP). However, many Medicare Advantage plans include dental coverage (which is not an included benefit under Original Medicare). Yet others include reimbursement for taxi rides to physician appointments, optometry exams, and annual gym memberships. If choosing to enroll in a Medicare Advantage plan, the enrollee still needs to pay the monthly cost of Original Medicare’s Part B – even though those covered services are already included in the Medicare Advantage plan.
Comparing the cost of different Medicare Advantage Plans
Monthly premiums and annual deductible costs differ tremendously between Medicare Advantage plans. While there are plans with no monthly premiums at all, these often have higher annual deductibles. More than 4,000 Medicare Advantage plans nationwide were offered to seniors in 2023. Since the CMS rates Medicare Advantage plans for enrollee satisfaction on a scale of 1-5 (as well as Part D drug plans), checking the CMS “star” rating for a Medicare Advantage plan can help a senior to determine whether to enroll in that particular plan or a different one.
Supplemental (Medigap) Plans, Part D Plans, and Travel Health Insurance
Due to the diverse costs accruable to people enrolled in Original Medicare, many seniors enrolled in Medicare’s Parts A, B, and D choose to also buy supplemental (Medigap) insurance. This is offered by private insurance companies, and can cover the deductibles and co-insurance not normally covered by Original Medicare. The monthly cost of a Medigap plan varies, but generally depends upon how much of the uncovered costs will be paid by the Medigap plan. As of 2018, 34% of people covered by Original Medicare purchased supplemental (Medigap) insurance. (If enrolled in a Medicare Advantage plan, the CMS disallows simultaneous enrollment in a Medigap plan.)
Similar to the diversity of Medicare Advantage and Medigap plans, there are a huge number of Part D drug plans offered by private insurance companies to seniors. The determination of which is best depends upon the financial circumstances, usual daily medications, and pharmacy preferences of the senior. Monthly premiums and annual deductibles differ between Part D drug plans, and the cost of a monthly prescription of a specific drug can also differ widely between plans.
For a senior that lives for a few months each year somewhere other than the state of permanent residential address, Original Medicare may be preferable. On the other hand, a senior taking a three-week vacation overseas – especially if afflicted with a chronic health condition such as diabetes – may find that purchasing travel insurance (which is not included in Medicare coverage) may be a good idea.
Telehealth coverage and medicare
Consequent to the federal Covid-19 public health emergency declaration, telehealth “virtual” medical visits are covered by Medicare through December 31, 2024. Many Medicare Advantage plans have broader coverage for utilizing telehealth than Original Medicare. Additionally, an ever greater number of Medicare Advantage plans are covering the cost of digital devices and wearables for patient monitoring and telehealth visits. Since the CMS does not include language in its Original Medicare parameters that expressly covers digital health technology, a Health News article in 2023 concludes that such technology is more likely to be covered by Medicare Advantage plans than Original Medicare.
Consider purchasing the Ōmcare Home Health Hub® to enable remaining in the home environment in later life, rather than relocation to a Skilled Nursing Facility (SNF) or elsewhere.
How telehealth can cut your healthcare expenses
Providing health insurance to employees costs businesses, but so do preventable chronic health disorders leading to excessive absenteeism and/or lost productivity. Businesses in the US with 50 employees or more are required to offer health insurance to them or face federal tax penalties. Meanwhile, research findings published in Preventing Chronic Disease in 2016 noted that annual absenteeism costs ranged from $16 - $81 per employee for a small employer, and $17 - $286 per employee for a large employer. For this reason (and many others), managing healthcare-related expenditures is vital for businesses in order to remain profitable. Increasing employee access to telehealth is a strategy that can aid businesses to reduce employee healthcare service needs while curbing business healthcare expenditures.
Unhealthy employee lifestyles and the link to increased business healthcare costs
Obesity, smoking, and alcohol abuse are all widely recognized to be damaging to health. Among the 23% of all employed adults who smoke, 37% smoke 20 or more cigarettes each day. Obesity, smoking, and alcohol abuse are all linked to a significantly increased risk for heart attack (per the American Heart Association). Additionally, alcohol abuse is a contributing factor for obesity. Besides heart disease (a leading cause of disability and premature death), obesity, smoking, and alcohol abuse all are linked to a heightened risk for diabetes (Type 2).
The average (mean) cost for hospitalization due to heart disease is $10,737 - $17,830 per hospitalization (according to an article in 2022 in the Journal of Managed Care & Specialty Pharmacy). The annual cost for the treatment of solely diabetes in an adult afflicted with diabetes (Type 2) is around $9,601. Therefore, enabling employees to receive health education and participate in health prevention workshops via telehealth to address unhealthy lifestyles that can lead to a chronic disorder – which can then result in disability that increases workplace absenteeism – makes good sense for a business.
For the large number of employees living with diabetes (Type 2), utilizing telehealth in combination with digital health devices can promote better diabetes control. In turn, this can prevent worsened overall health and the development of such diabetic complications as neuropathy (nerve pain) and kidney failure.
Group health insurance rates for businesses and employee healthcare utilization
The annual rate that a business pays for group health insurance is largely determined by the insurers’ prediction of the costs associated with healthcare utilization (by employees of the business) that will be borne by the insurer. This is also the case for disability insurance rates. Therefore, businesses that have a high percentage of employees with diagnosed chronic health disorders (such as diabetes or hypertension) are more likely to be charged a higher annual rate for group health insurance (as well as disability insurance) coverage. This is yet another reason that preventing employees from developing chronic disorders is important for curbing annual business expenses.
The Milken Institute reported in 2018 that the following are the most expensive chronic health conditions in terms of national direct costs:
- Diabetes ($189.6 Billion in total)
- Alzheimer’s disease ($185.9 Billion in total)
- Osteoarthritis ($115.5 Billion in total)
Mental health distress is also linked to the development of chronic health disorders (as well as an increased risk for workplace injury and overall lowered productivity). Therefore, enabling employees at increased risk for a diagnosed mental health disorder to talk to a therapist is an excellent strategy to curtail related healthcare service costs. By reducing the need for employees to travel to appointments with clinicians (requiring a greater time period away from the workplace than a telehealth visit), maintaining usual workplace routines and overall productivity is more likely.
Lowered cost of telehealth versus in-person physician office visits
Insurance billing for an in-person office visit can be for more than just the visit with the physician or other clinician. A “facility fee” may be charged if the physician does not own the facility (and this is a common practice among hospital-run outpatient offices). In contrast, telehealth visits do not incur this added cost. However, a primary reason that telehealth can result in lowered healthcare expenditures by businesses is that acquiring help from a healthcare provider via telehealth for an illness/injury experienced by an employee while not at work (such as in the home environment) is more likely to lead to taking the correct action to prevent it from worsening.
For example, an employee who has sprained an ankle may learn through a telehealth appointment (using videoconferencing software) that applying ice right away and then wrapping the ankle with an ace bandage can speed up healing. In this way, the employee may not need to remain away from the workplace to heal for as long as otherwise. Likewise, an employee unsure of whether to take a daily medication with (or without) food can acquire an answer utilizing telehealth, rather than incorrectly taking the drug and consequently developing an untoward symptom.
Digital devices that keep track of glucose level, heart rate, sleep quality, daily calorie intake, and prescribed medication adherence – and that enable a person’s healthcare provider to receive the recorded data – can be combined with telehealth visits to maintain (and improve) health.
Contact Ōmcare to learn more about our digital health solutions, and how these can help your business.