The pill puzzle: Why current medication adherence isn’t enough
Around 125,000 deaths each year in the US are due to prescription medication non-adherence. The term – adherence – refers to following physicians’ prescription drug instructions to patients in treating their disorders. While a reported 50% of all patients struggle with medication adherence, this problem is even worse in seniors. One reason is a lack of understanding for the need to take a particular drug, but another is forgetfulness. However, that forgetfulness is most often related to taking multiple daily medications and mixing them up. Regardless of the specific reason for stopping a medication, confusion over when to take it, or never taking it at all, a chronic health disorder is likely to worsen as a result.
Prescription medications used to treat cancers: Why adherence is necessary
Oral chemotherapy pills that can be taken at home are replacing intravenous (IV) chemotherapy delivered in treatment centers for many patients. Four types of cancer that can now be treated by taking daily oral chemotherapy medications are:
- Leukemia
- Breast cancer
- Prostate cancer
- Renal cancer
According to the National Cancer Institute (NCI), half of all cancers occur in people aged 66 and older. Likewise, the NCI notes that senior age is the most important (overall) risk for cancer, with the median age linked to the following cancers:
- Breast cancer – median age at diagnosis: 62 years old
- Colorectal cancer – median age at diagnosis: 67 years old
- Prostate cancer – median age at diagnosis: 66 years old
When chemotherapy pills are suddenly discontinued or taken incorrectly, the cancer tumors can return or grow. An article in the Journal of Oncology Practice reported that three other consequences of chemotherapy pill nonadherence are increased use of healthcare resources, higher hospitalization rates, and longer inpatient stays. Especially for seniors with cancer, longer hospitalizations are linked to developing hospital-acquired infections.
Diabetes medication adherence in seniors and nonadherence consequences
At least 16.5 million adults aged 65 and older in the US are living with Type-2 diabetes, and many take oral prescription medication to control it. When the daily pill to control blood glucose level is skipped or taken at the wrong time of day, there is a far higher likelihood that diabetes complications will develop. These complications include neuropathy (nerve pain), heart disease, and kidney failure.
What is polypharmacy and why does this lead to medication nonadherence?
Polypharmacy is the term used to describe taking more than five different prescription drugs each day. Problematically, polypharmacy was reported in up to 39% of all adults aged 65 and older (per an article in Global Health Research and Policy). Meanwhile, short-term memory problems increase with aging. Therefore, the pill puzzle can become highly complex for seniors as they age. Since adults are living to much later ages than ever before, the generally low level of prescription medication adherence among adults needs to be increased. Otherwise, a lower overall quality of health after age 70 may be the consequence.
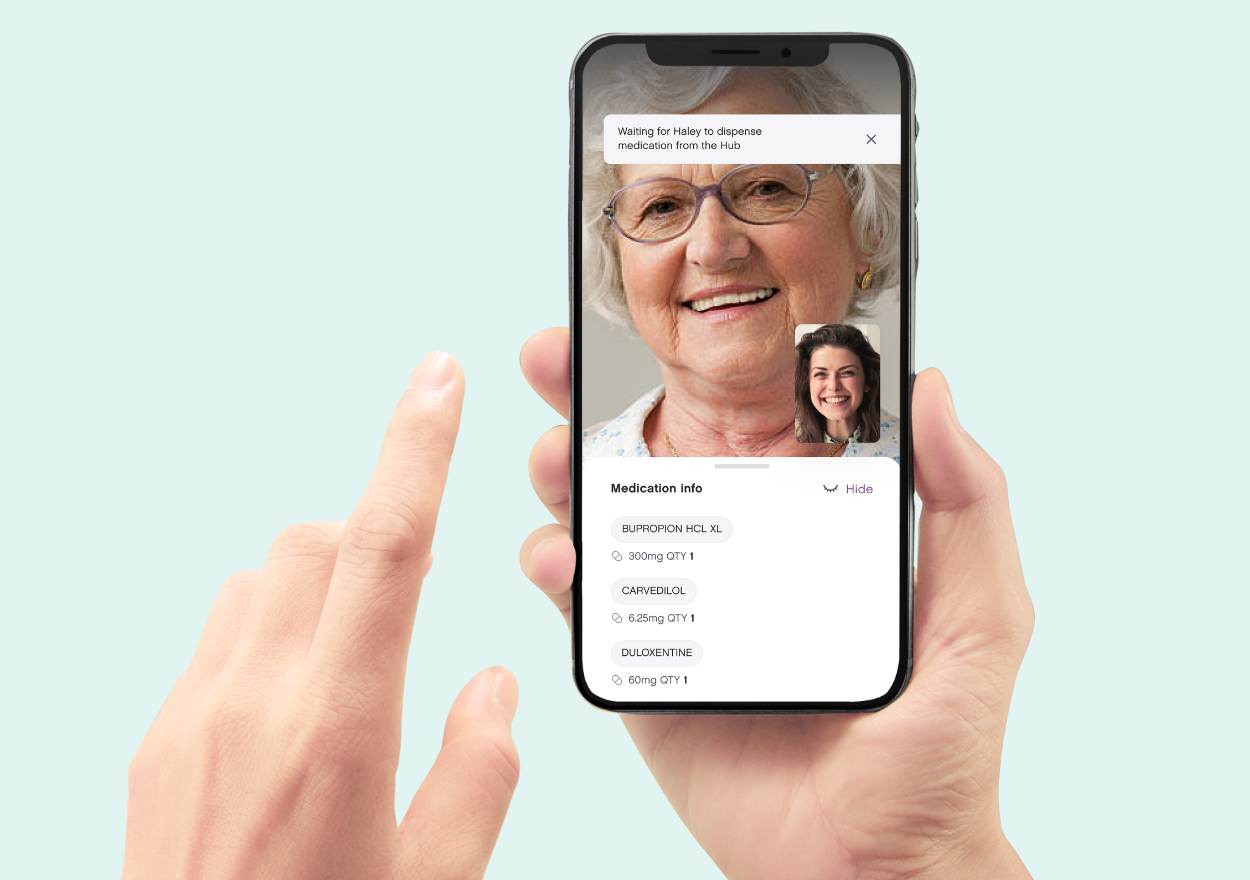
Digital devices, like the Ōmcare Home Health Hub® make guessing a thing of the past with medication reminders and one-touch access to video conferencing, guaranteeing right med, right time, right person every time.
The adherence advantage: Unlocking the benefits of enhanced medication adherence
Taking medications as prescribed is something that is not as easy as it sounds. This is especially the case for seniors, who may take several prescribed drugs each day. It really is vital to recognize that non-adherence can mean not taking a prescribed drug at all, or it can mean taking it but mixing up the dose or time of day to take it. The following describes what can happen if you do not take specific prescription drugs as prescribed, as well as the benefits of medication adherence to treating three common health disorders in seniors.
Lack of medication adherence in seniors with high blood pressure: Why it matters
Around 60% of all adults in the US by age 60 have high blood pressure (hypertension). This percent increases with age. Meanwhile, high blood pressure is the leading cause of strokes. Certain medications are prescribed to ensure that blood pressure remains within a normal range in adults living with chronic hypertension. In this way, a stable blood pressure is maintained, so as not to be too high or too low.
When a person skips a daily blood pressure medication, the result can be a dangerous spike in blood pressure. However – if a morning dose is taken instead at bedtime – the person could arise to use the bathroom, but then faint due to an overly-low blood pressure. This is because it can take several hours for an oral blood pressure drug to work as intended.
Medical researchers have determined that adults who are non-adherent to prescribed drugs to control hypertension are nearly six times more likely to have a stroke than those who are adherent. Since strokes often cause permanent disability in older-aged adults, adhering to blood pressure drugs can be imperative to future overall health and well-being.
The benefits of medication adherence for managing diabetes-type 2
At least 29% of all adults aged 65 and older are living with Diabetes-Type 2, per the Centers for Disease Control. While insulin is the standard treatment for Diabetes-Type 1, prescribed pills of antihyperglycemic drugs are the standard treatment for Diabetes-Type 2. These daily antihyperglycemic medications help to maintain the blood sugar level within normal range. If not taken each day (or not taken at all), the blood sugar level can remain too high or even increase.
Uncontrolled or poorly-controlled Diabetes-Type 2 can boost the likelihood of developing many of the common diabetes complications. These complications include:
- A type of nerve pain in the limbs called peripheral neuropathy
- Heart disease, resulting in an increased risk of heart attacks
- Blindness due to diabetic retinopathy
- Transient Ischemic Attacks (TIAs)
- Kidney damage
Benefits of medication adherence for controlling cholesterol level
High cholesterol increases the risk for a heart attack. According to the American Heart Association, the main reason is that too much cholesterol in the bloodstream causes fatty deposits (plaques) to form in the artery walls. In turn, the plaques can break off, travel in the bloodstream toward the heart as a clot, and then block blood-flow to the heart.
The FDA approved the first statin drug to lower cholesterol in 1987. Since that time, statins have been prescribed by doctors to many millions of adults to lower cholesterol. This is because taking a daily statin drug has been shown to tremendously lower heart attack risk in adults with chronically-high cholesterol. However, statin medication needs to be taken daily for life after beginning its use. Otherwise, cholesterol level is likely to spike back up.
Heart disease is the leading cause of death in adults in the US, and especially in senior-aged adults. Therefore, medication adherence to a prescribed statin drug by an adult diagnosed with high cholesterol can be life-saving.
How smart technology can increase medication adherence in seniors
Having a family member or friend remind a senior-aged person to take daily prescribed medications every day can be effective at increasing medication adherence to prescribed drugs. However, this is not a realistic solution in most cases, as even a family member or friend can forget to tell the senior-aged person every day to take the prescribed medication. Fortunately, there now are apps and other mobile devices that enable users to set reminders.
Meanwhile, voice-activated technology gadgets can also provide a medication reminder. While not specifically designed for seniors, these can be used by senior-aged adults. More recently, home-based smart devices have been developed that provide medication reminders. Notably, this can enable the user to be reminded each day to take a specific prescription medication at a specific time of day. Since these reminders can enable senior-aged adults to take daily medications at the right dose and at the right time of day, they can significantly increase medication adherence in seniors.
The Ōmcare Home Health Hub® is an all-in-one platform that is designed specifically for seniors and provides medication alerts while actually storing and dispensing the medication in pre-packaged pouches from the pharmacy, making right med, right time, right person a concern of the past.
Telehealth tips for caregivers: Supporting aging loved ones
Senior-aged adults often rely on adult children and other family members for home-based assistance. This can range from housecleaning to helping with bathing and dressing. There are at least 44 million “friends and family” unpaid caregivers in the US, and these caregivers are critical to the survival of homebound seniors. If you are a family member or friend performing a caregiving role to an elderly person, taking time away from that role to lower your caregiving stress can be a major challenge. Telehealth utilization can reduce that stress, as the need to drive your elderly loved one to frequent healthcare or allied therapy appointments can be eliminated. Moreover, it can also enable the senior-aged person to meet with a doctor or allied therapist (such as a physical therapist) to acquire health-related information without the need for an “in-person” appointment.
Below are three tips for caregivers to promote telehealth utilization by senior-aged loved ones:
Tip #1: Make sure the room is as quiet as possible during a telehealth session
One in every three people aged 65-74 has hearing loss. For those aged 75 and older, most have noticeable hearing loss. For seniors with age-related hearing loss, high and low-pitched voices can be the most difficult to hear clearly. Since the majority of hearing aids “work” by amplifying all nearby sounds, a loud television in the room during a telehealth session may prevent a hearing-impaired senior from understanding a doctor’s answers to questions. Therefore, it is vital to ensure that the room where the senior-aged person is located is as quiet as possible during the telehealth session. In this way, it is more likely that your senior-aged loved one will be able to get medical questions answered and feel comfortable using telehealth to interact with healthcare providers.
Tip #2: Have adequate lighting in the room where the telehealth visit will occur
Healthcare providers typically need to be able to see a patient in order to assess that person’s overall state of health. This is especially the case for senior-aged patients living with a chronic disorder, as worsening health can often be visible by viewing the face. For example, an unusual yellowish skin tone or jaundice in a person is common in those experiencing liver damage. If that jaundice has worsened – which happens in worsening liver damage – a person’s doctor may notice this during a telehealth visit, and determine an emergency “in-person” appointment is needed.
Furthermore, good lighting during a telehealth session can prevent a senior-aged person from developing eyestrain, which can result in your loved one stopping a telehealth session prematurely before getting the needed medical information.
Tip #3: Check the technology to ensure it works before the telehealth visit begins
It can be frustrating to discover that a computer’s webcam does not work during a telehealth visit with a healthcare provider. Likewise, internet connections can sometimes become unstable due to inclement weather events such as thunderstorms. According to AARP, two in five adults over age 65 feel that technological devices were not designed with them in mind.
Problematically, when a senior-aged person is unable to keep a telehealth visit because of a technology problem, that person is far more likely to not want to use telehealth again. Then, this unfortunate decision can result in your return to driving or escorting your senior-aged loved one to numerous healthcare providers’ offices. In turn, the negative result can be deciding not to keep those needed medical appointments.
Try teaching your loved ones or doing a practice call ahead of time.
These are just three tips to enhancing how a senior can use telehealth for better health and allow caregivers more peace of mind and time away. What else would you add to the list?
Technology in senior care: Enhancing the lives of caregivers and residents alike
Although many seniors would prefer to stay in their home, a sudden permanent disability can quickly require 24/7 home-based care that can be too expensive or just unavailable. Fortunately, technological solutions now exist that can enable seniors to continue to live independently or in assisted living residences rather than require relocation to a nursing home.
High tech home living and cleaning devices: An aid for seniors plus their caregivers
From technologically-controlled window shades to robotic vacuum cleaners, technology is enabling daily living activities and chores to be more easily accomplished. According to the US Census Bureau, 40% of adults aged 65 and older have at least one disability, of which 66% have difficulty in walking. Owning high tech home gadgets can simplify (and expedite) daily routines. In this way, the senior living independently or in an assisted living residence can maintain more personal independence than otherwise likely.
Videoconferencing technology and its impact on senior health
The widespread adoption of videoconferencing by seniors occurred largely due to the Covid-19 pandemic. As telehealth services began to replace in-person physician office visits during the height of the Covid-19 pandemic, more senior-aged people began to use videoconferencing apps. Through checking in with their doctors and other caregivers via this technology, many seniors were able to manage illnesses and chronic disorders without an in-person visit to do so. In particular, using a videoconferencing app on a Smartphone or computer has enabled seniors to interact with:
- Primary care providers such as physicians and nurse practitioners;
- Physical therapists and nutritionists;
- Psychologists and mental health counselors;
- Family members and friends
Through using telehealth and/or contacting family members online, preventive action to lessen progression to worsened health outcomes was enabled. For example, seniors who had fallen and sprained a knee or ankle could acquire input as to how to treat that sprain to improve faster healing. Thus, a longer period of time for that healing to occur – or a permanent joint disability resulting from improper self-treatment – could be avoided.
Telemedicine linking doctors to specialists: Why this matters for seniors
Many senior-aged people live with heart disease, diabetes (Type-2), kidney disease, or have experienced a stroke. In order to best treat and manage these types of chronic health disorders, primary care doctors typically refer their patients to specialists. For example, cardiologists are heart specialists who can tailor the treatment of a person’s heart disease to their underlying heart disorder and needs. Technological advances in telemedicine are enabling primary care doctors to link online with specialist physicians such as cardiologists to better coordinate their patients’ care.
Whether you are a senior-aged adult or someone caring for a senior, the Ōmcare Home Health Hub® is a technological device that can enable videoconferencing with personal and professional caregivers and managing daily medications. Thus, it can improve safe living in the home or in an assisted living facility.
Medication adherence 101: Why it matters and how to stay on track
The risk of a health disorder worsening is increased by non-adherence to treatment, most often seen as prescription medication non-adherence. Understanding the importance of taking medication as prescribed and implementing strategies to do so helps improve health outcomes.
According to the Centers for Disease Control, non-adherence is associated with higher rates of hospital admissions, worsened health, and an increased mortality (death) risk. Around 50% of all US adults are non-adherent to their prescribed medications. Meanwhile, seniors are the least likely to adhere to medication as prescribed by their doctors.
How medication adherence can impact managing acute and chronic health disorders
The dose of a medication is prescribed for each drug, as well as the drug itself. That dose is determined based on many patient factors, such as:
- Severity of the health disorder to be treated.
- Age of the patient.
- Body Mass Index (BMI) of the patient.
- Time of day a drug in pill form will be taken.
If a person prescribed a specific drug takes it at a lower or higher dose, the drug can be ineffective at treating the disorder or cause side effects. For example, some prescription medications to control high blood pressure (BP) are taken twice per day. If the patient takes it only once each day, the high BP may not be well-controlled. In turn, this could result in a preventable stroke.
Failure to take a prescribed drug – or suddenly stopping it – can lead to negative health effects.
Reasons seniors can fail at medication adherence
Nearly 40% of all adults experience some degree of short-term memory loss after age 65. Senior-aged adults are also more likely to take more daily prescription medications. This is because senior-aged adults are more likely to be afflicted with various chronic health disorders.
Some common chronic health disorders are also linked to an increased risk for depression based on brain chemistry changes. Researchers have found that depressed patients are 76% more likely to be non-adherent to prescribed medications as compared to their non-depressed counterparts. Whatever the reason for the non-adherence, there are methods you can use to stay on better track with your prescribed daily medications.
How prescription drug reminder messages can improve medication adherence
Setting an alarm on an alarm clock is one way to remind yourself to take a prescribed daily medication, many adults do this in order to take a particular prescription drug at a specific time. For seniors transferred from a hospital to a rehab center, the nursing staff will most likely let patients know when to take a prescribed medication and provide it to them. However, patients discharged at home are often left feeling hopeless with managing a complex schedule.
“Smart” digital devices such as Ōmcare’s Home Health Hub® are growing in popularity, due to their ability to provide reminders as well as enable videoconferencing. The Hub is specifically designed for seniors, and it can dispense the prescribed medication in pre-packaged pouches, as well as remind the senior to take it at exactly the right time.
Connecting generations: The role of telehealth in senior care
Mobility problems are far more common among senior-aged adults (as opposed to younger ones). At least 35% of seniors between 70-79 years of age, and most seniors aged 85 and older, have walking difficulties. Meanwhile, driving ability is also lessened among this age group. Fortunately, widespread telehealth expansion consequent to the Covid-19 pandemic has made it possible for more seniors to keep their scheduled medical appointments than ever before. While the overall benefits of using telehealth became obvious during the Covid-19 pandemic, the continued increase in telehealth use among seniors is enabling far better self-management of their chronic health conditions. From high blood pressure to diabetes, telehealth is helping more senior-aged patients to prevent worsening of their disorders through obtaining ongoing follow-up care. The following describes three of the vital roles of telehealth in senior care.
Telehealth for health prevention education
More than 50% of adults aged 65 and older are living with prediabetes, and 25% have full-blown Type-2 diabetes. For those diagnosed with prediabetes, changing daily eating habits right away may prevent the progression to Type-2 diabetes. Yet, eating a diet high in carbohydrates and/or sugar may be a lifelong habit that feels impossible to change. Furthermore, some people do not understand how changing daily eating habits can prevent Type-2 diabetes.
After prediabetes is diagnosed by a doctor, it is important to learn how to control blood sugar through daily dietary intake. While an appointment with a nutritionist or diabetes educator may be scheduled by the doctor that diagnosed the prediabetes, many seniors do not attend such appointments due to lack of transportation. However, being offered the option to attend these appointments “virtually” via telehealth can enable the person with prediabetes to change daily eating habits to avoid needing diabetes medication.
It is important to realize that a lack of understanding regarding how to prevent a particular chronic disorder is often the reason an older-aged person develops that disorder. For example, lack of a regular exercise routine increases the risk for heart disease. Notably, receiving health education by a nurse or doctor that is targeted toward increasing daily exercise in seniors can lead to better heart rate function. By undertaking a daily exercise routine, premature heart disease progression can be delayed in seniors experiencing the early symptoms of heart disease. Therefore, telehealth for health prevention education can enable seniors to prevent avoidable disabilities and premature death.
Managing medication refills through senior telehealth use
Skipped doses of medications account for 125,000 deaths annually, and 10-25% of hospital admissions. A common reason that seniors may skip prescribed doses is that they were not able to travel to pick up the next monthly supply of the medication from their pharmacy. Another is that those seniors needed to acquire a new refill prescription from the doctor in order for the pharmacy to continue providing that medication. By using telehealth, a senior may be able to quickly talk to their doctor and/or pharmacist to avoid running out of the medication. While many pharmacies can now deliver a patient’s medication to the home address, a current prescription refill request from a doctor still needs to exist at that pharmacy for it to be filled. Thus, telehealth can enable a rapid resolution of the problem that prevented the senior from having enough medication “on hand” not to skip a dose.
Recognizing when an “in-person” healthcare visit is necessary or not
Not every senior who is experiencing a symptom of a health disorder needs to have an “in-person” medical appointment to obtain treatment. Falls are the leading cause of injury in seniors, and one in every four seniors report a fall each year (per the Centers for Disease Control). While a fall can result in a broken bone, most falls just result in a sprained ankle or wrist. Talking to a healthcare provider via telehealth can enable the injured senior to care for the sprain at home in many cases.
This self-care may involve applying an ice pack, elevating the affected limb, and/or bandaging the joint in a specific way to prevent moving it. By having a healthcare provider instruct the senior-aged patient in how to self-treat a minor sprain via a telehealth visit, a trip to the doctor’s office (that could potentially further injure the joint) may be avoided. Meanwhile, following the healthcare provider’s self-care instructions may also promote faster healing of that sprain.
Senior-aged adults living with Type-2 diabetes and taking diabetes medication can sometimes have a sudden drop in blood glucose level. Most often, this is because a meal was skipped or the diabetic person engaged in unusually vigorous exercise. Through talking to a healthcare provider quickly via telehealth, the senior-aged person can find out how whether drinking some orange juice may be enough to reverse the low blood glucose (hypoglycemia) or whether injectable glucagon is necessary. Moreover, that telehealth visit can enable the diabetic senior to know whether to immediately visit a hospital Emergency Room for treatment.
The Ōmcare Home Health Hub® offers videoconferencing capabilities with loved ones and professional caregivers currently and will offer full telehealth abilities in the future. This allows the Hub to not provide medication reminders and dispensing of pre-packaged medications, but also will enable you to connect with a provider as well. Creating an all-in-one system makes using technology that much simpler and thus more effective.
Breaking barriers: Overcoming challenges in medication adherence
Less than 50% of all adults aged 60 and older are adherent to their prescribed medications (and the number goes way down when medication regimes increase in complexity). When drugs are prescribed to patients to treat disorders, the doses are tailored to that individual’s health needs. Therefore, not taking medications as prescribed (called nonadherence) can have dire consequences.
While in-person supervision all day to ensure that an older-aged person correctly takes their medications is effective, it is not possible for both cost and resourcing concerns. Fortunately, there are other options to overcoming challenges to medication adherence that also enable more personal independence.
Reminding yourself or your family member to adhere to prescribed medications
Reportedly, 40% of those aged 65 and older have short-term memory impairments, per a medical research article in BMJ.
Therefore, using some system to remind yourself (or your senior-aged loved one) to take a daily medication is a good idea. This is especially true for seniors who are taking multiple daily prescribed medications to manage chronic health disorders or prevent them from developing.
For inexpensive ways (yet not fully fool proof either), you could try daily planners, sticky notes, or cell phone reminders. However, keep in mind these tactics can have limitations — such as remembering if the sticky note was for today or yesterday.
Medication interactions and side effects: Their role in prescription drug nonadherence
The use of multiple daily medications to treat diseases and chronic health disorders is termed polypharmacy, according to the National Institute on Aging. This situation is most common in senior-aged people, and it increases the risk of a negative medication interaction. Around 50% of all seniors daily utilize at least five different medications. Meanwhile, a recent article in Cancer reported that 80% of senior-aged adults with cancer take five or more prescription drugs every day.
The potential for a negative drug-to-drug interaction – and especially a gastrointestinal (GI) effect such as constipation or diarrhea – can lead to nonadherence in taking prescribed medications. Meanwhile, there is a recognized relationship between polypharmacy and the risk for kidney damage in elderly people. Therefore, it is crucial that medication monitoring by healthcare providers occur on a frequent and regular basis in seniors taking multiple daily medications. In this way, seniors prescribed drugs to treat their chronic health disorders will be less likely to either stop or incorrectly take their medications.
Besides cancer, three common disorders in seniors that can require taking multiple daily prescribed medications are:
- Heart disorders (and especially following a heart attack resulting in heart damage)
- Stroke
- Diabetes (Types 1 and 2)
Why are seniors at greater risk for short-term memory problems?
Younger brains have a higher capacity for neuroplasticity than older brains. This means that – when brain cells mature and die – new ones are more likely to be generated at a more rapid rate in younger people than in senior-aged adults. Even more problematic, around 75% of all strokes occur in adults aged 65 and older. While a mild stroke may cause only slight weakness in a body part, strokes cause the death of brain cells. As a result, senior-aged stroke survivors are more likely to have short-term memory impairments.
Taking antidepressants over many years can also result in short-term memory loss (per an article in Psychiatry Journal). Since stroke survivors often experience chronic depression, antidepressants are often prescribed to them. Furthermore, dementia is far more common in seniors than younger aged adults. Whatever the cause, having a short-term memory impairment can lead to forgetting to take a prescribed daily medication.
The harmful consequences of not taking a prescribed medication
Disability is the most common consequence of not taking a prescribed medication or not taking it correctly. For example, diabetes that is not well-controlled can lead to diverse other health disorders. Peripheral nerve pain and heart disease are far more common in diabetics with poorly-controlled blood sugar than in those with their diabetes under good control.
Premature fatality is also a potential harmful consequence for people with chronic disorders who fail to take their daily medications. This is especially the case for people living with heart disease, cancer, or diabetes. Therefore, understanding why a specific medication is important plus not forgetting to take it is important for future health.
If you are a senior or the caregiver of a senior, the Ōmcare Home Health Hub® is an all-in-one platform that can aid medication adherence by both providing medication reminders and dispensing the prescribed medications in a pre-packaged pouch.
Beyond the prescription refill: Strategies for medication success in older adults
Most pharmacies provide reminders by phone or email to their customers to pick up a needed refill of a daily prescribed drug. That’s great, but it does not solve the problem for older-aged adults of remembering to take a daily medication and take it correctly. Indeed, around 50% of all seniors prescribed medication to manage their disorders do not take them as prescribed. Besides forgetting to take a prescribed pill, taking them at the wrong time of day or mixing them up altogether also occurs.
The following are some alarming statistics to consider about older-aged adults’ medication use. At least 90% of all seniors in the US take at least one prescribed daily medication, and 36% take five or more different ones each day. Meanwhile, up to 96% of seniors report that they frequently make mistakes in taking their prescribed drugs (per an article in 2019 in Expert Review of Clinical Pharmacology).
How to lessen the likelihood of forgetting which daily medication to take
Many prescribed pills look quite similar. However, some are of a different color, have indented areas in order to cut them, or have the pharmaceutical manufacturer’s name carved into them. Yet others are rectangular rather than round, or are in capsule or gummy form. Creating a poster to tape to your bedroom wall of a photo of each pill – with its name plus its corresponding instructions for use – is one strategy that can aid you (or your loved one) in telling those daily medications apart. This can take time to create, but it can be especially useful for people who put their pills in some type of pill box organizer.
Rather than placing all daily pills in a single (small) pill box, using a large pill box organizer with separate compartments for each day of the week can be an excellent strategy. However, the correct pill still has to be placed in the correct compartment. By taking a photo of each medication with its description (pasted onto a poster board that is taped to a wall), a dropped pill that lands on the kitchen table can be more easily identified to place it back in the correct compartment.
Using digital devices as a reminder tool for taking medications
Smartphones and other digital devices can be set up to provide a reminder on-screen to take your daily medication. In a recent study focused on people diagnosed with epilepsy, 71% reported using their cell phones to remind them to take their daily medication. Writing down each pill to be taken each day into a desk “calendar” (that includes a line for each hour of the day) may appear to be best for senior-aged people that do not know how to use smartphones or tablets. However, that manual method typically requires far more time and mental concentration to maintain correctly. Furthermore, it can result in accidentally writing the medication reminder on the wrong date and/or on the wrong calendar line corresponding to the time of day to take each pill.
A better strategy includes using all-in-one home health devices that can store your medications, take pictures, serve up pictures on each medication, and send reminders.
That’s exactly what the Ōmcare Home Health Hub® does while providing smartphone updates and real-time reporting to loved ones and caregivers. This eliminates the burden of manual sorting, manual reminders, or needing multiple devices to put it all together.
However you go about it, increasing the ease of getting the right med at the right time is critical to patient comfort, quality of life, and safety.
Connecting rural communities to better healthcare through technology
Rural communities in the US are the least likely to have Internet connectivity. In particular, many rural areas lack broadband connectivity, which is the high-speed Internet capacity that exists in non-rural communities. According to the US Department of Agriculture, at least 22% of all rural communities lack broadband, as compared to only 1.5% of urban communities. As you probably are well aware, the reason that broadband is now so critical is that it is required for cell phone and mobile device Wi-Fi, web-browsing, video-streaming, and many other types of connections. Moreover, it enables users to have a constant Internet connection, rather than having to connect through a dial-up modem.
Why is broadband internet connectivity needed by healthcare providers?
Healthcare providers, hospitals, and healthcare systems depend upon having a broadband connection to accomplish numerous and diverse tasks, including the following:
- Share health data (such as share a hospital record with a patient’s outpatient physicians);
- Offer telehealth services to patients;
- Interact in groups with other healthcare providers via videoconferencing software;
- Quickly communicate with patients and each other via a mobile phone call or text message;
- Share large amounts of data with state public health departments (such as share data about in-patients in each hospital admitted monthly with a Covid-19 infection);
- Submit a new medication prescription or a “refill” request online to a pharmacy.
Changes that are enabling increased broadband internet access in rural communities
Various federal governmental executive orders have enabled funding for the infrastructure needed for broadband (“high-speed”) Internet connections. This includes installing the underground cables and nearby satellite towers required for broadband Internet connections. Federal grants and loans have been offered/provided to develop broadband infrastructure in rural populated areas.
However, a gap still remains between broadband Internet in the homes of rural community residents in the US as opposed to residents of cities. According to a Pew Research Center report in 2024, 73% of adults in rural communities now have broadband Internet at home, as compared to 77% of adults in urban areas and 86% of adults in suburban areas. Notably, that proportion for rural residents was only 58% in 2018.
The capacity to access telehealth services & why it matters for patient health
The advantage of having access to telehealth services was highlighted during the Covid-19 pandemic, when access to “in-person” care became limited. One reason was that healthcare providers were concerned about contracting a Covid-19 infection from patients, and another was that patients were concerned about contracting Covid-19 from a healthcare setting. Therefore, telehealth became widely embraced as a way that patients could receive healthcare services without leaving home. This was especially valued by senior-aged and/or immune-compromised adults, who are at increased risk.
The use of videoconferencing software for telehealth interactions between clinicians (such as doctors and mental health therapists) was embraced, and continues to be particularly beneficial to the following groups of people:
- Adults aged 65 and older;
- Adults with physical disabilities;
- Adults without access to transportation to travel to a healthcare provider’s office.
People who live in rural communities frequently live far from the nearest hospital and their healthcare providers. The National Rural Health Association reports that – for every 100,000 people in a rural area of the US – there are 39 physicians to serve them. This is a direct contrast to 53 in urban areas. Meanwhile, there are only 30 specialist physicians (such as cardiologists) in rural areas, as opposed to 263 in urban areas. Hospital closures in rural areas in the past few years have far outpaced hospital closures in urban and suburban areas of the US.
The link between lack of broadband internet and chronic health disorders
It is vital to realize that a lack of access to physicians/hospitals in rural communities is a reason that the residents of rural communities in the US have more chronic health disorders than those not living in rural regions. Since prevention and early treatment of chronic disorders (such as Diabetes-Type 2) are often delayed due to lack of physician access, healthcare researchers have concluded that the high prevalence of chronic disorders in rural residents is largely due to a lack of early prevention and treatment access. Therefore, broadband Internet to access telehealth can be a “super-determinant” of health, per the US Substance and Mental Health Services Administration (SAMHSA).
Digital options for connection
As innovation continues in the home health space, many companies are moving toward cellular or low internet requirements to make this burden less prevalent and better reach rural communities.
For example, while the Ōmcare Home Health Hub still requires internet to function currently, it is the lowest amount possible, allowing for a lower need by both the patient and provider.
Is AI taking the place of in-person medication reminders?
Artificial Intelligence (AI) is being used by healthcare providers to better understand the effectiveness of prescribed drugs to treat a health disorder. It is also being used to better understand whether an individual patient is likely to forget to take a prescribed drug. The problem of forgetting to take a prescribed daily medication (or take it correctly) has huge implications. This is especially so for seniors with chronic health disorders. For example, not taking daily blood pressure (BP) medication to control high BP can lead to a spike in BP. In turn, this can result in a stroke. Therefore, knowing which patients need medication reminders and/or are likely to fail to take their prescribed medications is critical.
How senior-aged adults typically receive in-person medication reminders
The following are four customary ways that seniors receive “in-person” reminders to take their prescribed daily medications:
- Reminder from a spouse or other family member living in the same home with the older-aged person.
- Visits and/or phone calls from a family member or other loved one.
- Follow-up phone calls to a patient from a primary care doctor and/or neighborhood drugstore to check whether that person is taking a specific prescribed medication.
- Reminders during a scheduled visit by a paid caregiver such as a home health aide.
Relying on other people for reminders at any age can be risky, but it can be especially unreliable for senior-aged adults. Problematically, at least 27% of senior-aged adults live alone, the majority have no nearby adult children, and many married elderly people have a spouse with dementia. The problem of forgetting to take prescribed drugs and/or not taking them as physician-instructed (termed nonadherence) is especially found in older-aged adults who take multiple medications, according to a Journal of Family Medicine and Primary Care article.
Can AI enable improved medication understanding and patient adherence?
It is widely recognized among Health Information Technology (HIT) researchers that the huge patient datasets used by Artificial Intelligence (AI) can determine far more rapidly than healthcare providers or medical researchers:
- Whether a specific medication is more likely to manage a chronic health disorder (such as high blood pressure) in patients based on characteristics such as age, when compared to a different drug.
- Whether patients with certain health disorders are more likely to forget taking a prescribed daily drug, take it at the wrong time of day, or take too many (or too few) daily doses.
- Whether patients with a past history of nonadherence to prescribed medication are more likely to be nonadherent to a new prescribed medication, as based on the reason for the past nonadherence.
How AI medication reminders powered are delivered to patients
An ever-increasing number of physician practices, healthcare systems, pharmacies, and insurance companies are utilizing AI-powered medication-reminder apps to contact patients. That contact is most often made to the recipient’s landline or smartphone in the form of an automated phone call. Meanwhile, smartphones and other digital devices can (and do) receive additional reminders via email and text, based on the patient’s preference.
The reason for the booming AI medication-reminder trend
The primary reason AI-powered medication reminders have caught on so quickly among clinicians, pharmacists, and insurers (such as Medicare Advantage plans) is that a tremendous amount of staff time and energy is required to deliver a personal medication reminder to every patient that needs these reminders. However – while automated medication reminders can improve patient medication adherence – an article in Preventive Medicine concluded that interactive medication reminders are the most effective at increasing medication adherence.
Unlike automated reminders, interactive reminders can enable patients to ask questions and receive immediate answers about their prescribed medications. Therefore, an increased utilization of AI-powered chatbots (that simulate conversation) to answer patients’ medication questions is occurring. In this way, senior-aged patients taking multiple daily medications are less likely to skip taking one of their daily pills, get their dosages mixed up, and not understand the importance of taking each of the medications for their overall health.
As an increasing percentage of senior-aged adults acquire smartphones and other digital devices, AI is likely to take the place of in-person medication reminders on the part of healthcare providers, pharmacies, and insurance companies. That is a good thing since many people – and especially senior-aged people – still do not receive the frequent medication reminders they need to ensure proper adherence.