Breaking barriers: Overcoming challenges in medication adherence
May 3, 2024Age Tech,Senior CareBlog
Less than 50% of all adults aged 60 and older are adherent to their prescribed medications (and the number goes way down when medication regimes increase in complexity). When drugs are prescribed to patients to treat disorders, the doses are tailored to that individual’s health needs. Therefore, not taking medications as prescribed (called nonadherence) can have dire consequences.
While in-person supervision all day to ensure that an older-aged person correctly takes their medications is effective, it is not possible for both cost and resourcing concerns. Fortunately, there are other options to overcoming challenges to medication adherence that also enable more personal independence.
Reminding yourself or your family member to adhere to prescribed medications
Reportedly, 40% of those aged 65 and older have short-term memory impairments, per a medical research article in BMJ.
Therefore, using some system to remind yourself (or your senior-aged loved one) to take a daily medication is a good idea. This is especially true for seniors who are taking multiple daily prescribed medications to manage chronic health disorders or prevent them from developing.
For inexpensive ways (yet not fully fool proof either), you could try daily planners, sticky notes, or cell phone reminders. However, keep in mind these tactics can have limitations — such as remembering if the sticky note was for today or yesterday.
Medication interactions and side effects: Their role in prescription drug nonadherence
The use of multiple daily medications to treat diseases and chronic health disorders is termed polypharmacy, according to the National Institute on Aging. This situation is most common in senior-aged people, and it increases the risk of a negative medication interaction. Around 50% of all seniors daily utilize at least five different medications. Meanwhile, a recent article in Cancer reported that 80% of senior-aged adults with cancer take five or more prescription drugs every day.
The potential for a negative drug-to-drug interaction – and especially a gastrointestinal (GI) effect such as constipation or diarrhea – can lead to nonadherence in taking prescribed medications. Meanwhile, there is a recognized relationship between polypharmacy and the risk for kidney damage in elderly people. Therefore, it is crucial that medication monitoring by healthcare providers occur on a frequent and regular basis in seniors taking multiple daily medications. In this way, seniors prescribed drugs to treat their chronic health disorders will be less likely to either stop or incorrectly take their medications.
Besides cancer, three common disorders in seniors that can require taking multiple daily prescribed medications are:
- Heart disorders (and especially following a heart attack resulting in heart damage)
- Stroke
- Diabetes (Types 1 and 2)
Why are seniors at greater risk for short-term memory problems?
Younger brains have a higher capacity for neuroplasticity than older brains. This means that – when brain cells mature and die – new ones are more likely to be generated at a more rapid rate in younger people than in senior-aged adults. Even more problematic, around 75% of all strokes occur in adults aged 65 and older. While a mild stroke may cause only slight weakness in a body part, strokes cause the death of brain cells. As a result, senior-aged stroke survivors are more likely to have short-term memory impairments.
Taking antidepressants over many years can also result in short-term memory loss (per an article in Psychiatry Journal). Since stroke survivors often experience chronic depression, antidepressants are often prescribed to them. Furthermore, dementia is far more common in seniors than younger aged adults. Whatever the cause, having a short-term memory impairment can lead to forgetting to take a prescribed daily medication.
The harmful consequences of not taking a prescribed medication
Disability is the most common consequence of not taking a prescribed medication or not taking it correctly. For example, diabetes that is not well-controlled can lead to diverse other health disorders. Peripheral nerve pain and heart disease are far more common in diabetics with poorly-controlled blood sugar than in those with their diabetes under good control.
Premature fatality is also a potential harmful consequence for people with chronic disorders who fail to take their daily medications. This is especially the case for people living with heart disease, cancer, or diabetes. Therefore, understanding why a specific medication is important plus not forgetting to take it is important for future health.
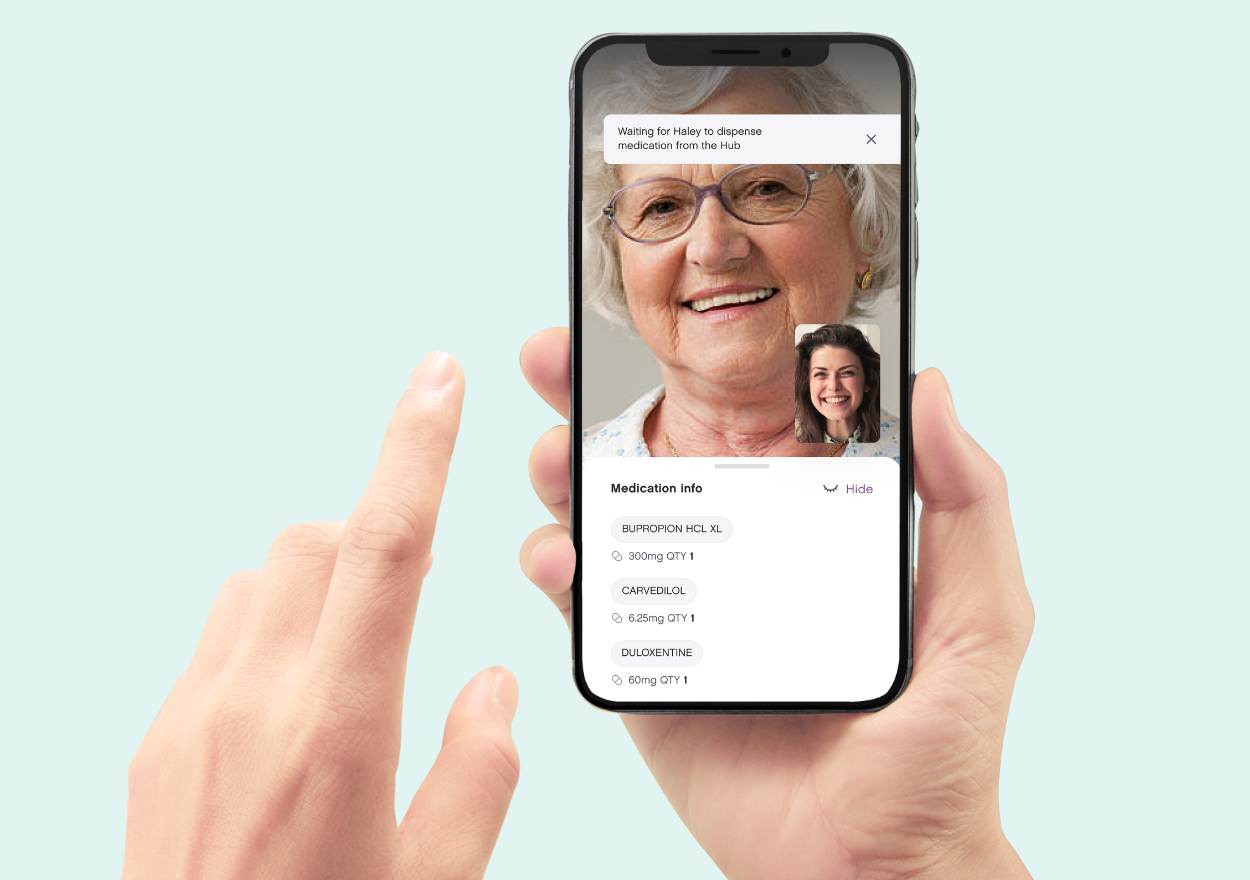
If you are a senior or the caregiver of a senior, the Ōmcare Home Health Hub® is an all-in-one platform that can aid medication adherence by both providing medication reminders and dispensing the prescribed medications in a pre-packaged pouch.
Beyond the prescription refill: Strategies for medication success in older adults
April 19, 2024Age Tech,Senior CareBlog
Most pharmacies provide reminders by phone or email to their customers to pick up a needed refill of a daily prescribed drug. That’s great, but it does not solve the problem for older-aged adults of remembering to take a daily medication and take it correctly. Indeed, around 50% of all seniors prescribed medication to manage their disorders do not take them as prescribed. Besides forgetting to take a prescribed pill, taking them at the wrong time of day or mixing them up altogether also occurs.
The following are some alarming statistics to consider about older-aged adults’ medication use. At least 90% of all seniors in the US take at least one prescribed daily medication, and 36% take five or more different ones each day. Meanwhile, up to 96% of seniors report that they frequently make mistakes in taking their prescribed drugs (per an article in 2019 in Expert Review of Clinical Pharmacology).
How to lessen the likelihood of forgetting which daily medication to take
Many prescribed pills look quite similar. However, some are of a different color, have indented areas in order to cut them, or have the pharmaceutical manufacturer’s name carved into them. Yet others are rectangular rather than round, or are in capsule or gummy form. Creating a poster to tape to your bedroom wall of a photo of each pill – with its name plus its corresponding instructions for use – is one strategy that can aid you (or your loved one) in telling those daily medications apart. This can take time to create, but it can be especially useful for people who put their pills in some type of pill box organizer.
Rather than placing all daily pills in a single (small) pill box, using a large pill box organizer with separate compartments for each day of the week can be an excellent strategy. However, the correct pill still has to be placed in the correct compartment. By taking a photo of each medication with its description (pasted onto a poster board that is taped to a wall), a dropped pill that lands on the kitchen table can be more easily identified to place it back in the correct compartment.
Using digital devices as a reminder tool for taking medications
Smartphones and other digital devices can be set up to provide a reminder on-screen to take your daily medication. In a recent study focused on people diagnosed with epilepsy, 71% reported using their cell phones to remind them to take their daily medication. Writing down each pill to be taken each day into a desk “calendar” (that includes a line for each hour of the day) may appear to be best for senior-aged people that do not know how to use smartphones or tablets. However, that manual method typically requires far more time and mental concentration to maintain correctly. Furthermore, it can result in accidentally writing the medication reminder on the wrong date and/or on the wrong calendar line corresponding to the time of day to take each pill.
A better strategy includes using all-in-one home health devices that can store your medications, take pictures, serve up pictures on each medication, and send reminders.
That’s exactly what the Ōmcare Home Health Hub® does while providing smartphone updates and real-time reporting to loved ones and caregivers. This eliminates the burden of manual sorting, manual reminders, or needing multiple devices to put it all together.
However you go about it, increasing the ease of getting the right med at the right time is critical to patient comfort, quality of life, and safety.
Connecting rural communities to better healthcare through technology
April 5, 2024Age Tech,Senior CareBlog
Rural communities in the US are the least likely to have Internet connectivity. In particular, many rural areas lack broadband connectivity, which is the high-speed Internet capacity that exists in non-rural communities. According to the US Department of Agriculture, at least 22% of all rural communities lack broadband, as compared to only 1.5% of urban communities. As you probably are well aware, the reason that broadband is now so critical is that it is required for cell phone and mobile device Wi-Fi, web-browsing, video-streaming, and many other types of connections. Moreover, it enables users to have a constant Internet connection, rather than having to connect through a dial-up modem.
Why is broadband internet connectivity needed by healthcare providers?
Healthcare providers, hospitals, and healthcare systems depend upon having a broadband connection to accomplish numerous and diverse tasks, including the following:
- Share health data (such as share a hospital record with a patient’s outpatient physicians);
- Offer telehealth services to patients;
- Interact in groups with other healthcare providers via videoconferencing software;
- Quickly communicate with patients and each other via a mobile phone call or text message;
- Share large amounts of data with state public health departments (such as share data about in-patients in each hospital admitted monthly with a Covid-19 infection);
- Submit a new medication prescription or a “refill” request online to a pharmacy.
Changes that are enabling increased broadband internet access in rural communities
Various federal governmental executive orders have enabled funding for the infrastructure needed for broadband (“high-speed”) Internet connections. This includes installing the underground cables and nearby satellite towers required for broadband Internet connections. Federal grants and loans have been offered/provided to develop broadband infrastructure in rural populated areas.
However, a gap still remains between broadband Internet in the homes of rural community residents in the US as opposed to residents of cities. According to a Pew Research Center report in 2024, 73% of adults in rural communities now have broadband Internet at home, as compared to 77% of adults in urban areas and 86% of adults in suburban areas. Notably, that proportion for rural residents was only 58% in 2018.
The capacity to access telehealth services & why it matters for patient health
The advantage of having access to telehealth services was highlighted during the Covid-19 pandemic, when access to “in-person” care became limited. One reason was that healthcare providers were concerned about contracting a Covid-19 infection from patients, and another was that patients were concerned about contracting Covid-19 from a healthcare setting. Therefore, telehealth became widely embraced as a way that patients could receive healthcare services without leaving home. This was especially valued by senior-aged and/or immune-compromised adults, who are at increased risk.
The use of videoconferencing software for telehealth interactions between clinicians (such as doctors and mental health therapists) was embraced, and continues to be particularly beneficial to the following groups of people:
- Adults aged 65 and older;
- Adults with physical disabilities;
- Adults without access to transportation to travel to a healthcare provider’s office.
People who live in rural communities frequently live far from the nearest hospital and their healthcare providers. The National Rural Health Association reports that – for every 100,000 people in a rural area of the US – there are 39 physicians to serve them. This is a direct contrast to 53 in urban areas. Meanwhile, there are only 30 specialist physicians (such as cardiologists) in rural areas, as opposed to 263 in urban areas. Hospital closures in rural areas in the past few years have far outpaced hospital closures in urban and suburban areas of the US.
The link between lack of broadband internet and chronic health disorders
It is vital to realize that a lack of access to physicians/hospitals in rural communities is a reason that the residents of rural communities in the US have more chronic health disorders than those not living in rural regions. Since prevention and early treatment of chronic disorders (such as Diabetes-Type 2) are often delayed due to lack of physician access, healthcare researchers have concluded that the high prevalence of chronic disorders in rural residents is largely due to a lack of early prevention and treatment access. Therefore, broadband Internet to access telehealth can be a “super-determinant” of health, per the US Substance and Mental Health Services Administration (SAMHSA).
Digital options for connection
As innovation continues in the home health space, many companies are moving toward cellular or low internet requirements to make this burden less prevalent and better reach rural communities.
For example, while the Ōmcare Home Health Hub still requires internet to function currently, it is the lowest amount possible, allowing for a lower need by both the patient and provider.
Is AI taking the place of in-person medication reminders?
March 22, 2024Age Tech,Senior Care,Medicare AdvantageBlog
Artificial Intelligence (AI) is being used by healthcare providers to better understand the effectiveness of prescribed drugs to treat a health disorder. It is also being used to better understand whether an individual patient is likely to forget to take a prescribed drug. The problem of forgetting to take a prescribed daily medication (or take it correctly) has huge implications. This is especially so for seniors with chronic health disorders. For example, not taking daily blood pressure (BP) medication to control high BP can lead to a spike in BP. In turn, this can result in a stroke. Therefore, knowing which patients need medication reminders and/or are likely to fail to take their prescribed medications is critical.
How senior-aged adults typically receive in-person medication reminders
The following are four customary ways that seniors receive “in-person” reminders to take their prescribed daily medications:
- Reminder from a spouse or other family member living in the same home with the older-aged person.
- Visits and/or phone calls from a family member or other loved one.
- Follow-up phone calls to a patient from a primary care doctor and/or neighborhood drugstore to check whether that person is taking a specific prescribed medication.
- Reminders during a scheduled visit by a paid caregiver such as a home health aide.
Relying on other people for reminders at any age can be risky, but it can be especially unreliable for senior-aged adults. Problematically, at least 27% of senior-aged adults live alone, the majority have no nearby adult children, and many married elderly people have a spouse with dementia. The problem of forgetting to take prescribed drugs and/or not taking them as physician-instructed (termed nonadherence) is especially found in older-aged adults who take multiple medications, according to a Journal of Family Medicine and Primary Care article.
Can AI enable improved medication understanding and patient adherence?
It is widely recognized among Health Information Technology (HIT) researchers that the huge patient datasets used by Artificial Intelligence (AI) can determine far more rapidly than healthcare providers or medical researchers:
- Whether a specific medication is more likely to manage a chronic health disorder (such as high blood pressure) in patients based on characteristics such as age, when compared to a different drug.
- Whether patients with certain health disorders are more likely to forget taking a prescribed daily drug, take it at the wrong time of day, or take too many (or too few) daily doses.
- Whether patients with a past history of nonadherence to prescribed medication are more likely to be nonadherent to a new prescribed medication, as based on the reason for the past nonadherence.
How AI medication reminders powered are delivered to patients
An ever-increasing number of physician practices, healthcare systems, pharmacies, and insurance companies are utilizing AI-powered medication-reminder apps to contact patients. That contact is most often made to the recipient’s landline or smartphone in the form of an automated phone call. Meanwhile, smartphones and other digital devices can (and do) receive additional reminders via email and text, based on the patient’s preference.
The reason for the booming AI medication-reminder trend
The primary reason AI-powered medication reminders have caught on so quickly among clinicians, pharmacists, and insurers (such as Medicare Advantage plans) is that a tremendous amount of staff time and energy is required to deliver a personal medication reminder to every patient that needs these reminders. However – while automated medication reminders can improve patient medication adherence – an article in Preventive Medicine concluded that interactive medication reminders are the most effective at increasing medication adherence.
Unlike automated reminders, interactive reminders can enable patients to ask questions and receive immediate answers about their prescribed medications. Therefore, an increased utilization of AI-powered chatbots (that simulate conversation) to answer patients’ medication questions is occurring. In this way, senior-aged patients taking multiple daily medications are less likely to skip taking one of their daily pills, get their dosages mixed up, and not understand the importance of taking each of the medications for their overall health.
As an increasing percentage of senior-aged adults acquire smartphones and other digital devices, AI is likely to take the place of in-person medication reminders on the part of healthcare providers, pharmacies, and insurance companies. That is a good thing since many people – and especially senior-aged people – still do not receive the frequent medication reminders they need to ensure proper adherence.
Aging in the digital age: seniors and smart devices
March 8, 2024Age Tech,Senior CareBlog
Use of digital and other tech devices is commonplace among younger adults, but less so among seniors. However, this reality is changing, and largely due to the broad embracement of “Smart” devices. According to the Pew Research Center, 61% of adults aged 65 and older now own a Smartphone. While this is in comparison to 95% of adults aged 30-49 (plus 83% aged 50-64) the gap between Smartphone adoption among younger adults and seniors is rapidly shrinking. There are now actually a tremendous variety of “Smart” devices that can make life easier and safer for senior-aged adults. The following describes four of the categories of “Smart” devices that can be especially helpful to seniors in their daily lives.
Voice-activated digital and tech-driven devices
The ability to voice-activate digital devices can be a crucial aid for seniors, due to age-related health conditions that can limit finger dexterity or mobility. From turning on the overhead lights in the morning to unlocking the front door, voice-activated “Smart” devices such as Alexa and Google Assistant – paired with a Smart Home gadget – can simplify routine daily tasks. Six other tasks that this type of voice-activated device can do are:
- Let the device user know the day’s weather forecast;
- Turn on (and off) a coffee-maker, microwave oven, or robotic vacuum cleaner;
- Adjust the thermostats in the home to align with the desired temperature;
- Play selected music or an audio book;
- Add a food item to a digital list of groceries to purchase at a supermarket;
- Remind the user of a daily task to be performed such as picking up prescription medications from the drugstore
Around 47% of all adults aged 65 and older have diagnosed osteoarthritis (OA). Meanwhile, nearly 26% of senior-aged people have hand/finger OA. Therefore, voice-activated “Smart” devices can enable seniors living with OA to perform activities that would otherwise be far more difficult, if not impossible.
“Smart” medical alert systems
Medical alert systems that automatically dial 9-1-1, request an ambulance, and/or contact a patient’s doctor can be life-savers for senior-aged people. Three-fourths of all strokes occur in adults aged 65 and older, per a medical research article published in Aging. Without fast treatment, even a mild stroke can result in paralysis. Likewise, heart attacks require immediate medical intervention. For diabetics, a sudden spike in blood sugar level can necessitate obtaining an insulin injection to prevent slipping into a diabetic coma.
While medical alert systems – that paired a device similar to a landline telephone with a wristband (or neck pendant) containing an activation “button” – have existed since the 1980s, “Smart” alert systems now exist on most cell phones and many other types of digital devices.
Medication reminder and dispensing systems
It can be hard to remember to take a prescribed pill at any age, and this is particularly so for senior-aged adults. One reason that remembering to take prescribed medications can be more difficult for seniors is that adults aged 65 and older tend to take more daily pills than younger adults. More than half of all senior-aged adults take at least five daily prescription drugs. Telling those pills apart can be hard, and especially in elderly people with worsening eyesight or early Alzheimer’s disease. In turn, this can lead to a mix-up of taking too many pills each day of one prescribed medication and not enough of another.
While a medication reminder can be provided utilizing various “Smart” devices (such as a Smartphone), there are far fewer that can dispense the medications. The Ōmcare Home Health Hub® is one of those “Smart” devices that can dispense medications, as well as provide a reminder to take them.
“Smart” fitness trackers
Engaging in regular daily exercise is important for overall health, and this can be vital in senior-aged people to prevent heart disease. Notably, daily exercise has been found to ward off cognitive decline (such as short-term memory loss) in older-aged people. Mechanical devices such as pedometers have long been recommended to track steps per day.
However – ever since the first Fitbit was marketed to the public in 2009 – there has been an explosion in the availability of “Smart” fitness trackers. Not only have these been used by people (including senior-aged adults) while engaging in fitness activities, but they also have enabled their users to monitor heart rate, respiration rate, and blood pressure.
Overall, utilizing a “Smart” device can assist seniors in maintaining their personal independence, as well as boosting the likelihood of preserving health. Thus, this type of device can aid in reducing the likelihood of developing a preventable disability. By choosing the Omcare Home Health Hub, you can access its diverse capabilities that would otherwise require owning many different “Smart” devices.
The rise and fall of healthcare trends since the pandemic
February 21, 2024Age Tech,Senior CareBlog
Trends in healthcare are constantly changing to adapt to hospital, physician, and patient needs. The Covid-19 pandemic necessitated new ways of delivering patient care that reduced the likelihood of infecting clinicians and patients. Meanwhile, technological advances enabled the development of more collaborative approaches by physician teams to treat patients. However, no change happened so quickly and dramatically as the shift toward providing online “telehealth” services to patients (per a medical research article in 2020). The following describes three rising healthcare trends since the onset of Covid-19, and three healthcare system “norms” that are fading away.
Three rising trends in healthcare delivery to patients
- Increased adoption of team-based approaches to providing patient care:
The high cost of treating chronic disorders such as heart disease, Diabetes Type 2, and asthma has led public health leaders to promote healthcare provider team-based approaches to care. Likewise, the health complications commonly found in hospitalized Covid-19 patients after their discharge required more collaborative efforts.
For example, kidney damage was found in at least 30% of people hospitalized due to Covid-19. Without long-term physician care, daily medications, and dietary changes, people with kidney damage can progress to the life-threatening disorder of kidney failure. By enabling collaboration between primary care doctors (PCPs), specialist physicians, mental health therapists, and nutritionists, a post-hospitalization care approach for recovered Covid-19 patients with kidney damage could be quickly developed and implemented.
Videoconferencing software linking networks of healthcare providers boosted the capacity for healthcare teams to collaborate more efficiently. This continues to enable increased collaborative efforts, and is a rapidly-growing nationwide trend.
- Providing “telehealth” patient care as opposed to requiring a doctor’s office visit:
The use of videoconferencing software and digital solutions has exploded since the onset of the Covid-19 pandemic. Besides enabling people diagnosed with Covid-19 to interact with their healthcare providers without infecting them, telehealth visits also enabled outpatient clinicians to provide help each day to more patients. This was because there was no need to clean and re-stock an exam room for each new patient, since the interactions were conducted online. In addition, it eliminated the necessity for patients to travel to the healthcare provider’s office to receive care.
Elderly patients tend to have an especially difficult time in finding a way to travel to a healthcare provider’s office. Many people aged 70 and older either no longer drive or are unable to use public transportation to reach their healthcare provider’s office. This is especially problematic for seniors without any adult children living close to them, or who have physical disabilities that limit walking.
The huge advantage of “virtual” office visits is that it enables people to receive care from their clinicians without leaving home. Consequently, this has led to an expansion in the capacity of “virtual” technological solutions to deliver healthcare to patients. Not only have healthcare providers and patients embraced “virtual” visits since the onset of the Covid-19 pandemic, mental health therapists are hopping on the bandwagon in large numbers.
- The use of robotic devices to perform surgery:
While the first robotic device used to perform surgery was FDA-approved in the early 2000s, advances in robotic device mechanisms have led to increased usage of robotic devices to perform surgeries. This is especially the case for surgeries requiring finger dexterity beyond that normally possible for the human hand. Outside of use by the military in field hospitals, FDA-approved surgical robotic devices are most often utilized in hospital operating rooms to assist in performing minimally-invasive (laparoscopic) procedures. For example, in 2021, the Hominis Surgical System was approved by the FDA to perform transvaginal hysterectomies.
The use of robotic devices to perform surgical procedures has enabled surgeries to occur with just the presence of a surgeon and one or two assistants, rather than numerous Operating Room (OR) staff members. Therefore, the daily scheduling of more minimally-invasive surgeries per day by hospitals is possible. Due to its revenue-boosting potential, use of robotic devices to perform surgeries is an increasing trend that we imagine will only continue to rise.
Three falling (and disappearing) trends
- Short waiting times in hospital Emergency Rooms (ERs):
Healthcare staff “burn-out” is contributing to fewer personnel to assist patients who walk into a hospital Emergency Room (ER), rather than arriving in an ambulance. However, another reason waiting times are lengthening is that an increasing number of community hospitals are closing, with more people seeking ER care at the remaining hospitals.
- Manual healthcare billing systems:
Billing systems used in physician group practices that send out invoices manually are going the way of the dinosaur. In their place, technologically-driven systems, that can quickly identify correct billing codes and spot billing errors, are becoming a standard practice.
- Rapidly finding an available bed in a nursing home when needed:
Since 2016, more than 500 nursing homes have closed, and many more plan to do so. A chief reason specified by nursing home owners is that they simply cannot afford to stay in business. Meanwhile – as a consequence of the Covid-19 pandemic – it has also been harder for nursing homes to find and hire new nursing aides willing to work for low pay while risking a Covid-19 infection. Since a minimum staff-to-patient ratio is required by state governments, nursing homes cannot accept more patients than they have nursing aides on staff to care for them. Therefore, finding an available nursing home bed to take your elderly family member who can no longer safely live at home is taking far longer than in the past.
These are just some of the changed trends currently occurring across our healthcare system. Advances in Artificial Intelligence (AI) medical research, the development of mRNA cancer treatments, and the continuing shift toward value-based payments by both Medicare and private insurers are other trends that are gathering steam.
Among its numerous capabilities, the Ōmcare Home Health Hub® can enable you to engage in virtual healthcare visits as well as appointment/medication reminders and medication dispensing allowing home to be the site of care.
Employee Spotlight: Wendy Mizutani
February 13, 2024Employee SpotlightBlog
Name: Wendy Mizutani
Title: Vice President of Customer Care and Operations
Education: Master’s of Arts in Leadership, Augsburg University (graduating May 2024), Bachelor’s of Arts in Diplomacy and World Affairs, Occidental College
Time at Ōmcare: 4 Months (also 4 months end of 2019 and beginning of 2020)
One personal fact about you: My happy place is our family cabin in the mountains of Northern California.
1. What led you to Ōmcare?
When changing careers in 2019, I knew that I wanted to join the healthcare industry. In particular, I have a passion for helping people live independently as long as possible, based on my experiences as a caregiver for my mom. I met Lisa through a mutual connection and was inspired by Ōmcare’s mission of changing the way the world cares and addressing un-met needs for the growing population of adults 65+.
2. What’s the most rewarding part of working at Ōmcare?
Hearing from Hub owners, potential owners, and caregivers how Ōmcare simplifies their lives or takes a worry off their very full plate.
3. What is your favorite current project you’re working on?
I love working with the team to help deliver a product our customers will love and building a team of customer care professionals who share a passion to help.
4. Pick out a core value that means a lot to you. How have you seen this lived out in your time at Ōmcare?
We are a team. We understand the lifting power of many wings can achieve twice as much as any bird flying alone. Quite simply, there are no swim lanes or silos at Ōmcare. We’re here to help each other and everyone’s voice and contribution matter.
5. What are you most proud of accomplishing throughout your time at Ōmcare?
I really love the brand identity work that we’ve done with Marketing – it’s how we want to show up not only for our customers but for each other. It aligns with our values and mission and will become the way that we measure success and the quality of our customer service.
6. Why should someone work at Ōmcare?
Ōmcare is a company dedicated to making a real difference in the lives of our customers and their loved ones. Working for a company with clarity on their purpose matters and doing it with people who share that passion is invigorating. Ōmcare is a place where you can grow your skills and be valued for your experience, opinions, and hard work.
Is technology the cure for the loneliness epidemic?
February 9, 2024Age Tech,Senior CareBlog
Senior-aged adults experienced a loneliness surge during the height of the Covid-19 pandemic. Yet, even before the pandemic, 40% of adults over age 65 reported feeling lonely. This makes sense when we consider that social isolation is a major cause of loneliness in senior-aged adults. Despite fewer Covid-19 hospitalizations, the Covid-induced increase in social isolation continues to persist among senior-aged adults. Technology use was embraced by many seniors during the pandemic mainly due to its capacity to enable online interpersonal connections. Medical research findings published in 2022 confirmed this increased Internet and digital device utilization among the elderly due to the Covid-19 pandemic.
The causes of senior-aged social isolation
Nearly four in 10 senior-aged adults live with extended family worldwide. However, those in the US rarely do. As of 2020, 28% of community-dwelling seniors lived alone. While death of a spouse or dementia in a spouse are major reasons for increased social isolation among older-aged adults, an increased amount of disability and death among longstanding friends is another cause. The following are four other causal factors:
- Relocation by adult children to a new residence far from their senior-aged parents;
- Worsened eyesight, leading to reduced driving to engage in social interactions;
- Chronic health disorders and physical disabilities that limit visiting family and friends;
- Higher risk to contract an infection resulting from large social gatherings.
At least 50% of adults aged 60 or older are at risk for social isolation, with 33% expected to experience a high degree of loneliness in future, per a recent article in BMC Public Health. In turn, this reveals that a loneliness epidemic in senior-aged adults requires immediate attention.
The link between loneliness, depression, and chronic health disorders
Loneliness can lead to chronic depression in both younger and older adults. However, chronic depression in seniors is also strongly-linked to the development of the following chronic health disorders:
- High blood pressure;
- Heart disorders such as arrhythmia;
- Obesity;
- Alzheimer’s disease and other dementias
According to the National Institute of Mental Health, chronic depression also increases the risk for chronic pain. In addition, it increases the risk for sleep disorders such as insomnia. Notably, sleep disorders are linked to an increased risk for depression and numerous chronic health conditions. Most of all, chronic depression and sleep disorders both tend to lessen the brain’s release of certain biochemicals – such as Serotonin – that boost mood and stave off depression.
Mental health benefits of technology utilization in the elderly
At 70 years of age, two out of three adults in the US have some level of cognitive impairment, most commonly short-term memory deficits and worsened reflexes. Overall, mental health is worsened by cognitive impairments (such as decreased problem-solving capacity). Since chronic depression as well as diverse chronic health disorders can foster increased cognitive impairments, engaging in digital “brain health” activities in can be beneficial for preserving cognitive functioning.
Brain plasticity & technology use
Brain plasticity—meaning the capacity for creating new nerve pathways in the brain—boosts cognitive ability and overall brain health. While younger brains have a higher degree of brain plasticity, findings published in Frontiers in Aging Neuroscience have shown that the elderly can also boost their brain plasticity. This is a particular reason that learning new information and skills (such as the use of tech gadgets) is especially beneficial for the mental health of senior-aged adults.
Additionally, continuous learning activities have been clinically recognized as protective of cognitive functioning in senior-aged adults. Therefore, learning new technology programs and digital devices can aid elderly individuals to both preserve their level of cognitive function, as well as interrupt further cognitive decline.
How technology can address the loneliness epidemic
While technology by itself cannot “cure” the loneliness epidemic, it can certainly help. Senior quality-of-life can be improved by interacting with others via technological approaches, which can boost both mental/emotional well-being and overall health.
Videoconferencing programs and social media have enabled interpersonal communication to continue among adults living with disabilities that limit their capacity to attend “in-person” social activities. This is especially the case for disabled senior-aged people who can no longer venture far from home. In this way, technology utilization can both lessen social isolation and loneliness – thereby reducing the likelihood of worsened mental health and physical health.
Ōmcare not only serves as a medication reminder and telehealth interface, but it also connects seniors to loved ones with the simple touch of a button. To learn more about how we’re bringing health and connection into the home, visit omcare.com.
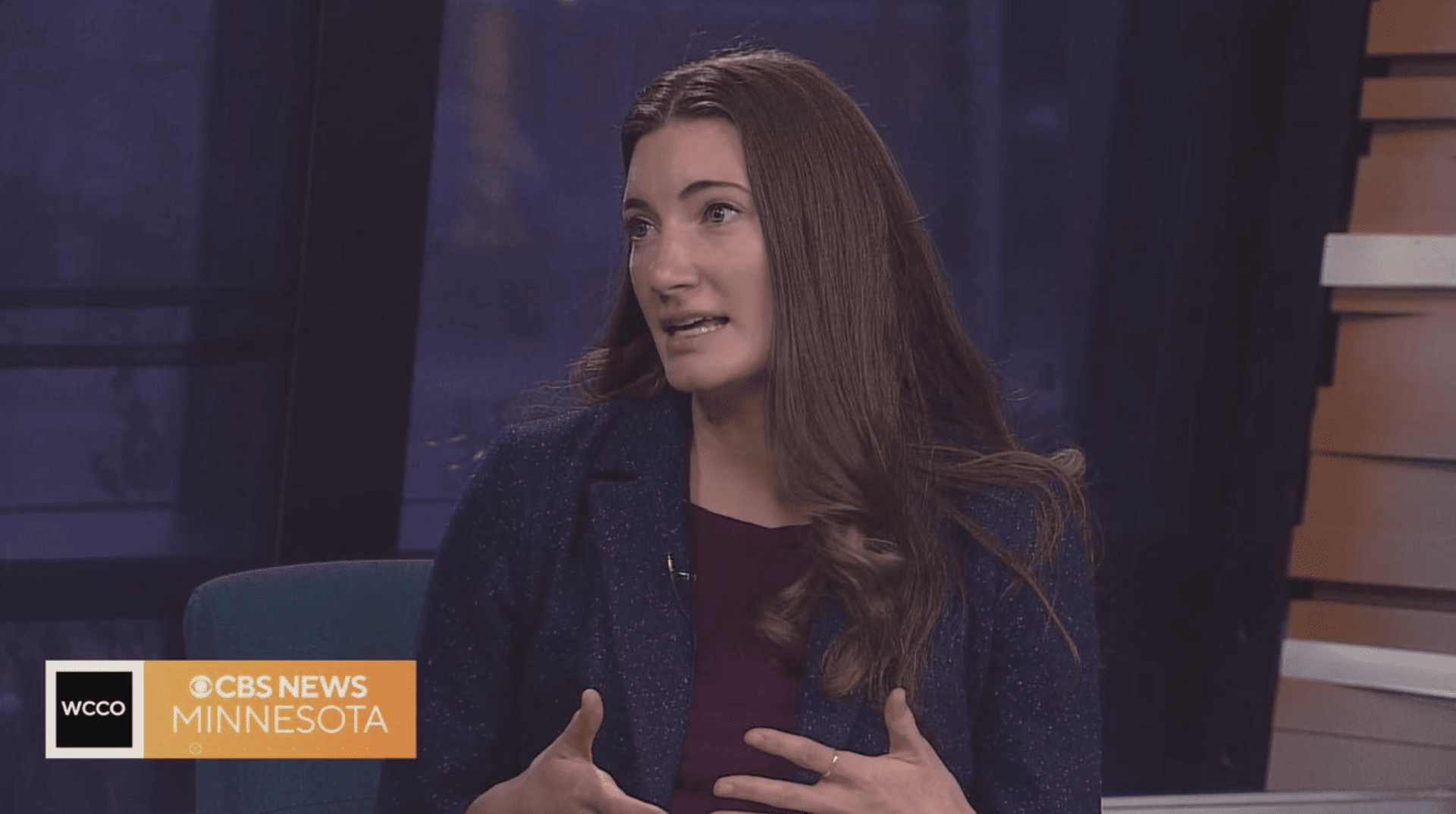
Ōmcare talks about the importance of monitoring your health with CBS News Minnesota, 1/29/24
National Self-Check Month stresses importance of regular health checks. Watch Morgan Rogers from Ōmcare talk about the importance of monitoring your health.
Watch the full news clip from CBS News Minnesota here.
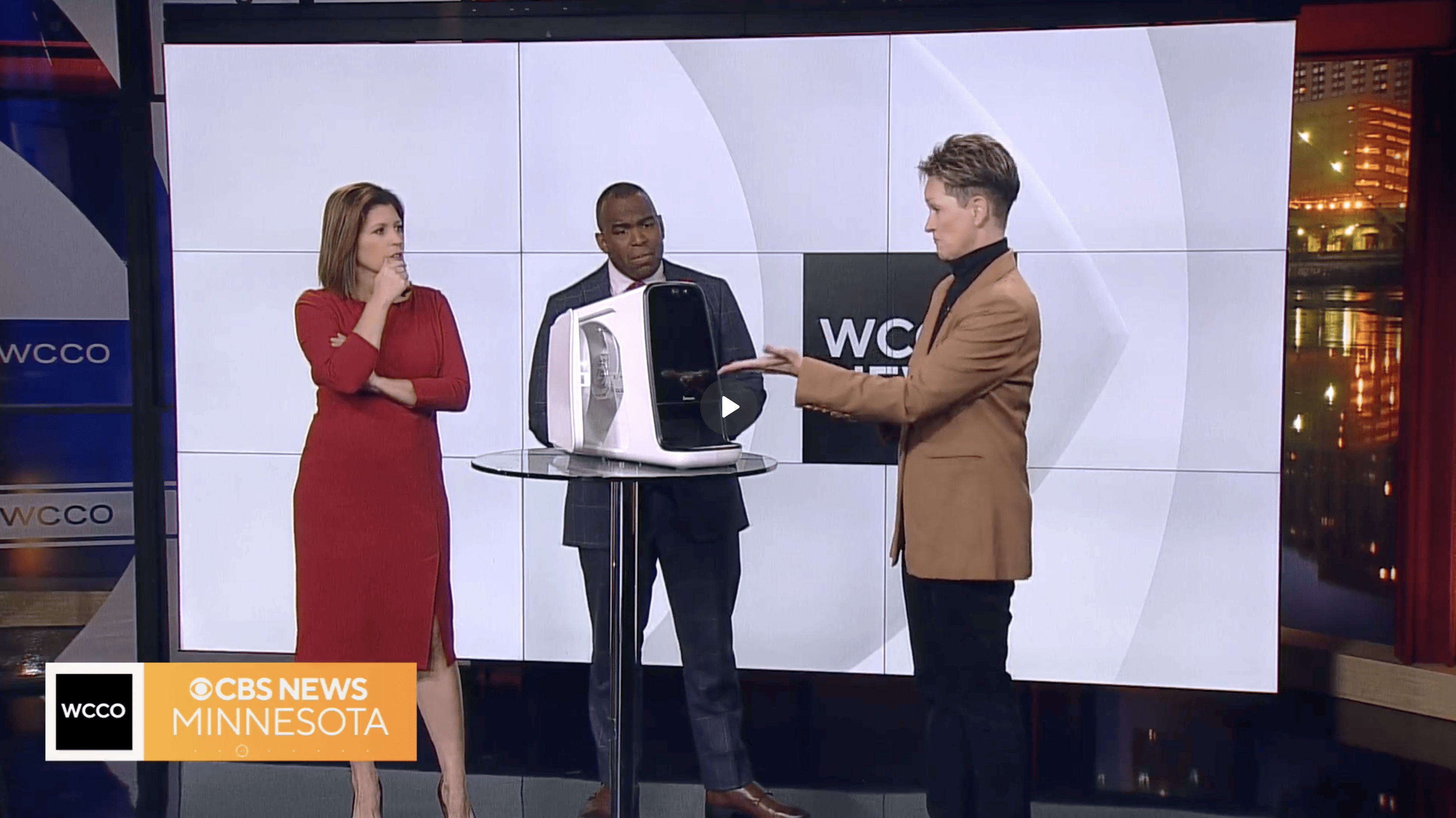
Ōmcare recognizes National Family Caregivers Month with CBS News Minnesota, 11/21/23
"Bloomington based Ōmcare wants to make the job of caregiver as easy as possible. CEO Lisa Lavin talks about how they're doing that."
Watch the full news clip from CBS News Minnesota here.