Ōmcare talks about how new technology helps seniors and caretakers stay on top of their meds with CBS News Minnesota, 6/29/25
For the many who are caregivers, doling out meds can be tricky. It can be tricky, too, for those trying to maintain their independence. In fact, medication mismanagement is the leading cause of hospitalizations among older adults.
Watch the full news clip from CBS News Minnesota here.
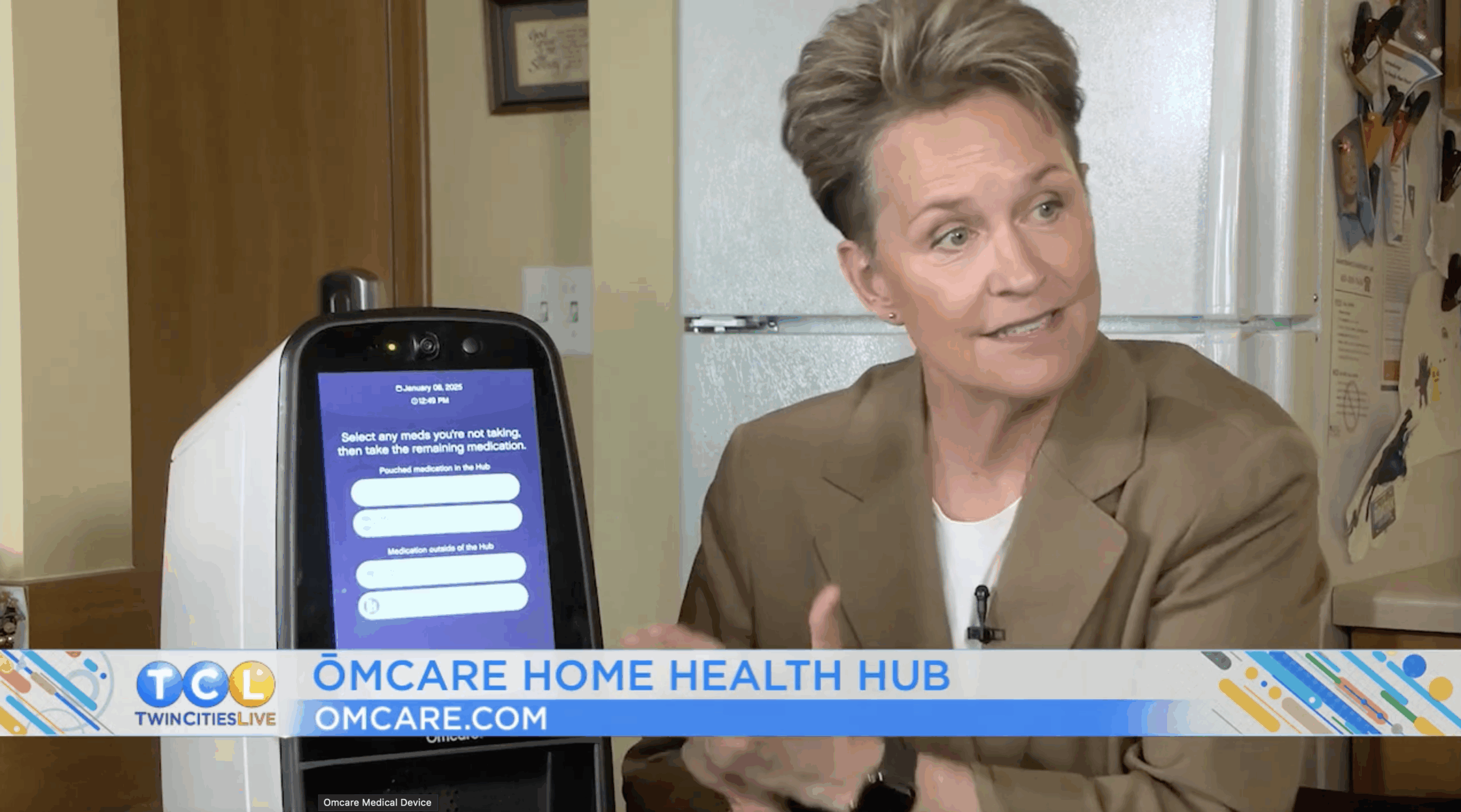
Ōmcare helps seniors keep track of their medicine and stay healthy with Twin Cities Live, 5/20/25
TCL Reporter Kelli Hanson introduces us to a device called Ōmcare that helps seniors keep track of their medicine and keeps them healthy.
Watch the full news clip from Twin Cities Live here.
Twin Cities Home Care Providers Launch Innovative In-Home Medication Assistance Service to Improve Health and Independence
May 5, 2025PressPress Releases,News
MINNEAPOLIS, MN – May 5, 2025 — Two leading Twin Cities home care agencies, CareAparent and Right at Home (Bloomington), have launched a new In-Home Medication Assistance Service, powered by the Ōmcare Home Health Hub®, to help aging adults stay healthier and live independently at home longer.
Medication mismanagement is the leading cause of hospitalization among older adults and a major contributor to loss of independence. With 80% of adults aged 65+ managing multiple prescriptions daily, timely and accurate adherence is essential.
Today, the responsibility of managing complicated medication routines often rests on family caregivers—most often an adult daughter or son. This role can require juggling multiple pharmacy visits, organizing pill boxes, tracking paper schedules, and providing daily oversight. These time-consuming and manual processes can erode the quality of the parent/child relationship and can lead to errors, often resulting in missed doses, confusion, and avoidable medical emergencies.
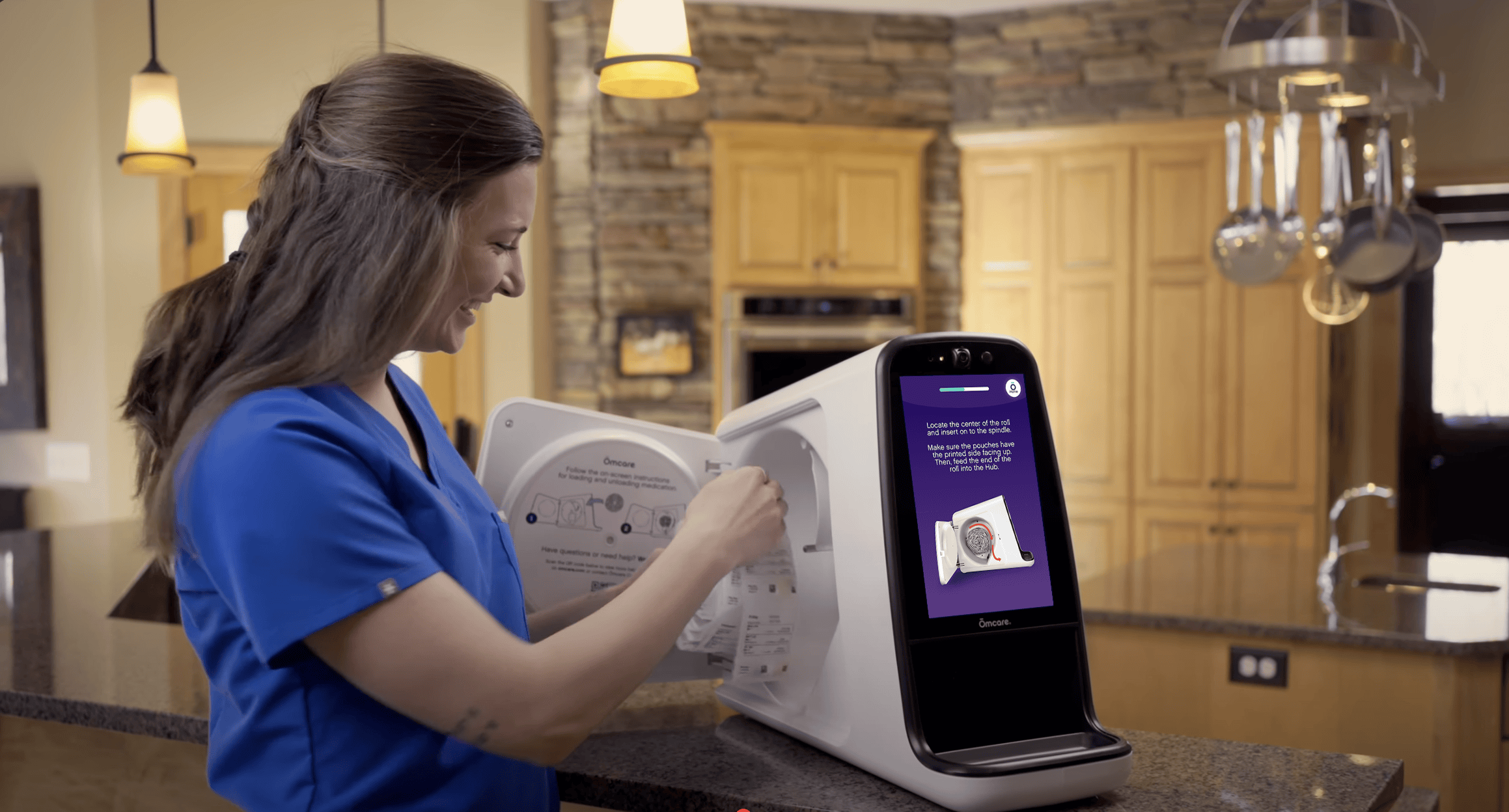
The new service is a comprehensive, turnkey solution designed to reduce medication errors and hospitalizations by supporting patients where they need it most—at home. It includes:
- Home-delivered, pouched medications from a national pharmacy
- Medication loading by trained home care professionals into the Ōmcare Home Health Hub®
- Automated alerts and dispensing when it’s time to take medications
- Verification of medication intake and real-time adherence tracking
- Easy one-touch video calls with family and caregivers
“This is exactly the kind of innovation we need in home care,” said Jody Hahn, CEO of CareAparent. “Medication adherence is one of the most critical components of healthy aging. The combination of human care and digital precision offers our clients greater peace of mind.”
“We’re proud to bring this transformative service to our clients and our community,” said Paul Blom, Co-Owner & CEO of Right at Home (Bloomington). “It aligns with our mission to Improve the Quality of Life for Those We Serve. Ōmcare will help us further empower individuals to age with dignity and independence, and it adds a new layer of safety and support.”
“At Ōmcare, our mission is to Change the way the world cares® for our aging population,” said Lisa Lavin, Founder and CEO of Ōmcare. “Everyone deserves the opportunity to live a vibrant, independent life—surrounded by connection, supported by care. We designed the Ōmcare platform to be a simple hub for health, connection, and wellbeing—empowering people to thrive in the place they call home.”
This groundbreaking service is now available to clients of CareAparent and Right at Home in the Twin Cities. Contact Ōmcare at 952-456-6848 or omcare.com/homecare to learn more.
___________________________________________________
About Ōmcare
Ōmcare is a digital health company that is Changing the way the world cares® for our aging population by seamlessly integrating innovative technology and compassionate service—making connection and care easier. Learn more at omcare.com/homecare
About CareAparent
CareAparent is a full-service home care provider in the Twin Cities. With a strong culture of hospitality and a genuine dedication to the people they serve, CareAparent is a supportive, responsive partner across the care journey. Contact CareAparent at https://careaparent.com/
About Right at Home
Right at Home Bloomington is a locally owned and operated in-home care agency offering personalized care plans for seniors who wish to remain in their homes. Their team is dedicated to improving quality of life and supporting families with trusted caregiving services. Contact Right at Home at https://www.rightathome.net/twin-cities
Ōmcare Debuts “Phygital” Home Health Platform at CES
December 11, 2024PressPress Releases,News
The Digital Health Technology Leader to Showcase How it’s Changing the Way the World Cares® for the Aging Population
MINNEAPOLIS (Dec. 10, 2024) – Ōmcare®, a Minnesota-based leader in digital health technology, will make its CES debut. The Ōmcare Home Health Hub® will showcase how it's transforming the way the world cares® for the aging population through its new “phygital” approach to remote healthcare at the world’s most influential technology event from January 7-11 in Las Vegas, NV.
More than 11,000 Americans turn 65-years-old every day, leaving more than 1 in 5 adults — a total of 53 million Americans — as unpaid family caregivers. For many, the journey of caring for aging loved ones can be challenging, both emotionally and financially. The Ōmcare Home Health Hub is giving caregivers the crucial support they need to help keep their aging loved ones in their own homes while helping them maintain their wellness and independence from afar.
Through its adaptive “phygital” approach to remote health management, the Ōmcare Home Health Hub seamlessly blends the physical aspects of health support with the benefits of digital connectivity. By linking patients, pharmacies and care providers with technology through its comprehensive, user-friendly system, the Ōmcare Home Health Hub fosters a sense of community and human connection while providing a holistic caregiving experience, ensuring aging individuals feel supported and connected at all times. The core system features include:
- Easy video calls available through a one-touch audiovisual system helping aging adults stay connected to their caregiving team at all times.
- Dispensing pouched medications direct from the pharmacy helping aging adults and their caregivers seamlessly and efficiently manage medication regimens.
- A three-camera system that enables visual confirmation of medication adherence, ensuring the right medication is taken at the right time.
- Biometric monitoring integration that offers a transparent view of the care recipient’s health.
“As caregiving options for aging loved ones grow increasingly scarce and the costs of in-home and facility care continue to rise, families are urgently seeking dependable and affordable solutions for essential needs like medication management,” said Lisa Lavin, CEO of Ōmcare. "For years, medication management has been a significant challenge for aging adults, with many struggling to manage complex regimens. This issue often leads to hospitalizations and a loss of independence. Ōmcare offers a breakthrough solution by directly integrating with pharmacy systems to automate medication scheduling and ensure timely, accurate dispensing. Our platform not only enhances adherence to prescribed medications, but also keeps caregivers informed and provides clear insights into their loved ones’ well-being, ensuring peace of mind for families."
The Ōmcare Home Health Hub was designed with accessibility in mind to meet the needs of older adults. Thoughtfully engineered, the system addresses solutions to common age-related challenges that can create barriers with in-home technology such as reduced vision and limited dexterity. By prioritizing design features such as intuitive functionality, visual clarity, enhanced screen sensitivity and high decibel sound, the platform is not only user-friendly but also highly accessible, empowering individuals to manage their care needs with confidence and ease.
Ōmcare will be exhibiting at CES as a portfolio company of AgeTech Collaborative™ from AARP, an unparalleled innovation ecosystem bringing together cutting-edge thinkers in the longevity tech space to champion meaningful advances so that everyone can choose how they live as they age. For more information about the Ōmcare Home Health Hub and its leading remote care technology, please visit Ōmcare.com.
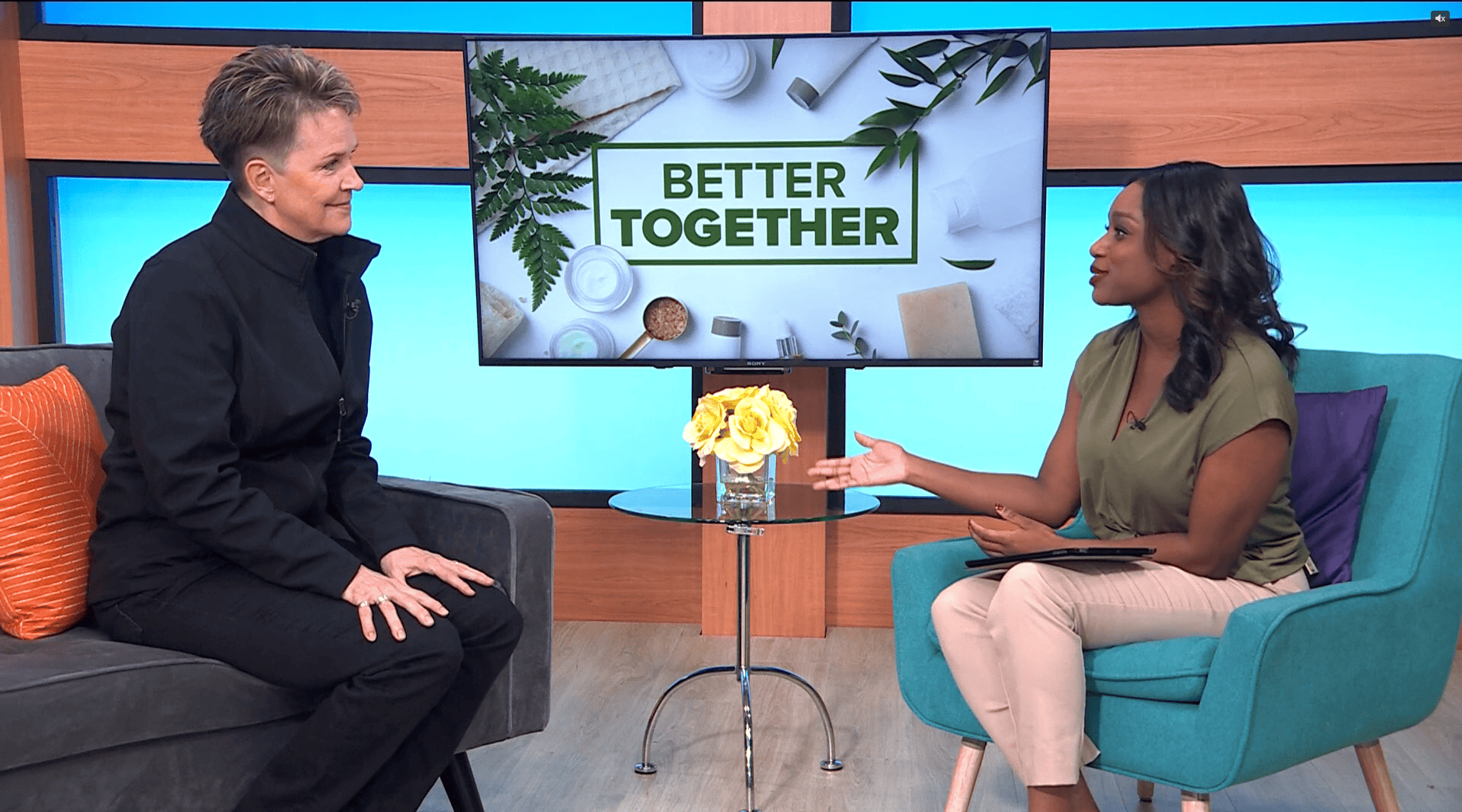
Lisa Lavin visits KARE 11 News at Noon to share more about Ōmcare and the shortage of caregivers in Minnesota, 11/27/24
About 1 in 5 Americans operate as an unpaid caregiver. This device could ease the labor.
The device includes remote care, video connection and medication dispensing so that caregivers are able to check in and care for their loved ones or patients virtually.
Lavin visited KARE 11 News at Noon to share more about Ōmcare and the shortage of caregivers in Minnesota.
According to AARP and the National Alliance for Caregiving, more than 20% of Americans were unpaid family caregivers in 2020. To ease the labor for caregivers, Minneapolis resident Lisa Lavin invented Ōmcare’s Home Health Hub device.
Watch the full news clip from Kare 11 here.
Ōmcare Appoints Healthcare Industry Veteran Martha Goldberg Aronson to its Board in preparation for scale
November 18, 2024PressPress Releases,News
MINNEAPOLIS, November 19, 2024 -- Today Ōmcare announced the appointment of Martha Goldberg Aronson to its Board of Directors. Martha is a distinguished healthcare industry leader with over 25 years of experience who brings extensive expertise in scaling medical device businesses.
"Martha's appointment to our board comes at a critical inflection point for Ōmcare as we prepare to scale," said Lisa Lavin, CEO of Ōmcare. "Martha’s proven ability to guide companies through rapid expansion while maintaining operational excellence makes her an ideal addition to our board. We look forward to benefiting from Martha’s leadership and expertise as we continue to revolutionize medication adherence and remote care delivery."
Ms. Goldberg Aronson currently serves as Chair of the Board for ConMed Corporation and comes with extensive board experience in medical technology. She has held executive leadership positions at several leading healthcare companies including Medtronic, Hill-Rom and Ecolab. During her tenure at Medtronic, she led the business unit that successfully launched the InterStim sacral neuromodulation device, demonstrating her ability to bring innovative medical technologies to market and scale operations effectively.
"I'm honored to join Ōmcare's Board of Directors at this important juncture," said Ms. Goldberg Aronson. "As our population continues to age, medication non-adherence and our caregiver shortage become even more pressing challenges. Ōmcare's innovative technology platform addresses these critical issues and supports an individual’s wellness and independence. I look forward to working alongside the board and management team to help scale this transformative platform and create meaningful impact for healthcare providers, patients, and their families.”
The pill puzzle: Why current medication adherence isn’t enough
July 26, 2024Age Tech,Senior CareBlog
Around 125,000 deaths each year in the US are due to prescription medication non-adherence. The term – adherence – refers to following physicians’ prescription drug instructions to patients in treating their disorders. While a reported 50% of all patients struggle with medication adherence, this problem is even worse in seniors. One reason is a lack of understanding for the need to take a particular drug, but another is forgetfulness. However, that forgetfulness is most often related to taking multiple daily medications and mixing them up. Regardless of the specific reason for stopping a medication, confusion over when to take it, or never taking it at all, a chronic health disorder is likely to worsen as a result.
Prescription medications used to treat cancers: Why adherence is necessary
Oral chemotherapy pills that can be taken at home are replacing intravenous (IV) chemotherapy delivered in treatment centers for many patients. Four types of cancer that can now be treated by taking daily oral chemotherapy medications are:
- Leukemia
- Breast cancer
- Prostate cancer
- Renal cancer
According to the National Cancer Institute (NCI), half of all cancers occur in people aged 66 and older. Likewise, the NCI notes that senior age is the most important (overall) risk for cancer, with the median age linked to the following cancers:
- Breast cancer – median age at diagnosis: 62 years old
- Colorectal cancer – median age at diagnosis: 67 years old
- Prostate cancer – median age at diagnosis: 66 years old
When chemotherapy pills are suddenly discontinued or taken incorrectly, the cancer tumors can return or grow. An article in the Journal of Oncology Practice reported that three other consequences of chemotherapy pill nonadherence are increased use of healthcare resources, higher hospitalization rates, and longer inpatient stays. Especially for seniors with cancer, longer hospitalizations are linked to developing hospital-acquired infections.
Diabetes medication adherence in seniors and nonadherence consequences
At least 16.5 million adults aged 65 and older in the US are living with Type-2 diabetes, and many take oral prescription medication to control it. When the daily pill to control blood glucose level is skipped or taken at the wrong time of day, there is a far higher likelihood that diabetes complications will develop. These complications include neuropathy (nerve pain), heart disease, and kidney failure.
What is polypharmacy and why does this lead to medication nonadherence?
Polypharmacy is the term used to describe taking more than five different prescription drugs each day. Problematically, polypharmacy was reported in up to 39% of all adults aged 65 and older (per an article in Global Health Research and Policy). Meanwhile, short-term memory problems increase with aging. Therefore, the pill puzzle can become highly complex for seniors as they age. Since adults are living to much later ages than ever before, the generally low level of prescription medication adherence among adults needs to be increased. Otherwise, a lower overall quality of health after age 70 may be the consequence.
Digital devices, like the Ōmcare Home Health Hub® make guessing a thing of the past with medication reminders and one-touch access to video conferencing, guaranteeing right med, right time, right person every time.
The adherence advantage: Unlocking the benefits of enhanced medication adherence
July 12, 2024Age Tech,Senior CareBlog
Taking medications as prescribed is something that is not as easy as it sounds. This is especially the case for seniors, who may take several prescribed drugs each day. It really is vital to recognize that non-adherence can mean not taking a prescribed drug at all, or it can mean taking it but mixing up the dose or time of day to take it. The following describes what can happen if you do not take specific prescription drugs as prescribed, as well as the benefits of medication adherence to treating three common health disorders in seniors.
Lack of medication adherence in seniors with high blood pressure: Why it matters
Around 60% of all adults in the US by age 60 have high blood pressure (hypertension). This percent increases with age. Meanwhile, high blood pressure is the leading cause of strokes. Certain medications are prescribed to ensure that blood pressure remains within a normal range in adults living with chronic hypertension. In this way, a stable blood pressure is maintained, so as not to be too high or too low.
When a person skips a daily blood pressure medication, the result can be a dangerous spike in blood pressure. However – if a morning dose is taken instead at bedtime – the person could arise to use the bathroom, but then faint due to an overly-low blood pressure. This is because it can take several hours for an oral blood pressure drug to work as intended.
Medical researchers have determined that adults who are non-adherent to prescribed drugs to control hypertension are nearly six times more likely to have a stroke than those who are adherent. Since strokes often cause permanent disability in older-aged adults, adhering to blood pressure drugs can be imperative to future overall health and well-being.
The benefits of medication adherence for managing diabetes-type 2
At least 29% of all adults aged 65 and older are living with Diabetes-Type 2, per the Centers for Disease Control. While insulin is the standard treatment for Diabetes-Type 1, prescribed pills of antihyperglycemic drugs are the standard treatment for Diabetes-Type 2. These daily antihyperglycemic medications help to maintain the blood sugar level within normal range. If not taken each day (or not taken at all), the blood sugar level can remain too high or even increase.
Uncontrolled or poorly-controlled Diabetes-Type 2 can boost the likelihood of developing many of the common diabetes complications. These complications include:
- A type of nerve pain in the limbs called peripheral neuropathy
- Heart disease, resulting in an increased risk of heart attacks
- Blindness due to diabetic retinopathy
- Transient Ischemic Attacks (TIAs)
- Kidney damage
Benefits of medication adherence for controlling cholesterol level
High cholesterol increases the risk for a heart attack. According to the American Heart Association, the main reason is that too much cholesterol in the bloodstream causes fatty deposits (plaques) to form in the artery walls. In turn, the plaques can break off, travel in the bloodstream toward the heart as a clot, and then block blood-flow to the heart.
The FDA approved the first statin drug to lower cholesterol in 1987. Since that time, statins have been prescribed by doctors to many millions of adults to lower cholesterol. This is because taking a daily statin drug has been shown to tremendously lower heart attack risk in adults with chronically-high cholesterol. However, statin medication needs to be taken daily for life after beginning its use. Otherwise, cholesterol level is likely to spike back up.
Heart disease is the leading cause of death in adults in the US, and especially in senior-aged adults. Therefore, medication adherence to a prescribed statin drug by an adult diagnosed with high cholesterol can be life-saving.
How smart technology can increase medication adherence in seniors
Having a family member or friend remind a senior-aged person to take daily prescribed medications every day can be effective at increasing medication adherence to prescribed drugs. However, this is not a realistic solution in most cases, as even a family member or friend can forget to tell the senior-aged person every day to take the prescribed medication. Fortunately, there now are apps and other mobile devices that enable users to set reminders.
Meanwhile, voice-activated technology gadgets can also provide a medication reminder. While not specifically designed for seniors, these can be used by senior-aged adults. More recently, home-based smart devices have been developed that provide medication reminders. Notably, this can enable the user to be reminded each day to take a specific prescription medication at a specific time of day. Since these reminders can enable senior-aged adults to take daily medications at the right dose and at the right time of day, they can significantly increase medication adherence in seniors.
The Ōmcare Home Health Hub® is an all-in-one platform that is designed specifically for seniors and provides medication alerts while actually storing and dispensing the medication in pre-packaged pouches from the pharmacy, making right med, right time, right person a concern of the past.
Telehealth tips for caregivers: Supporting aging loved ones
June 28, 2024Age Tech,Senior CareBlog
Senior-aged adults often rely on adult children and other family members for home-based assistance. This can range from housecleaning to helping with bathing and dressing. There are at least 44 million “friends and family” unpaid caregivers in the US, and these caregivers are critical to the survival of homebound seniors. If you are a family member or friend performing a caregiving role to an elderly person, taking time away from that role to lower your caregiving stress can be a major challenge. Telehealth utilization can reduce that stress, as the need to drive your elderly loved one to frequent healthcare or allied therapy appointments can be eliminated. Moreover, it can also enable the senior-aged person to meet with a doctor or allied therapist (such as a physical therapist) to acquire health-related information without the need for an “in-person” appointment.
Below are three tips for caregivers to promote telehealth utilization by senior-aged loved ones:
Tip #1: Make sure the room is as quiet as possible during a telehealth session
One in every three people aged 65-74 has hearing loss. For those aged 75 and older, most have noticeable hearing loss. For seniors with age-related hearing loss, high and low-pitched voices can be the most difficult to hear clearly. Since the majority of hearing aids “work” by amplifying all nearby sounds, a loud television in the room during a telehealth session may prevent a hearing-impaired senior from understanding a doctor’s answers to questions. Therefore, it is vital to ensure that the room where the senior-aged person is located is as quiet as possible during the telehealth session. In this way, it is more likely that your senior-aged loved one will be able to get medical questions answered and feel comfortable using telehealth to interact with healthcare providers.
Tip #2: Have adequate lighting in the room where the telehealth visit will occur
Healthcare providers typically need to be able to see a patient in order to assess that person’s overall state of health. This is especially the case for senior-aged patients living with a chronic disorder, as worsening health can often be visible by viewing the face. For example, an unusual yellowish skin tone or jaundice in a person is common in those experiencing liver damage. If that jaundice has worsened – which happens in worsening liver damage – a person’s doctor may notice this during a telehealth visit, and determine an emergency “in-person” appointment is needed.
Furthermore, good lighting during a telehealth session can prevent a senior-aged person from developing eyestrain, which can result in your loved one stopping a telehealth session prematurely before getting the needed medical information.
Tip #3: Check the technology to ensure it works before the telehealth visit begins
It can be frustrating to discover that a computer’s webcam does not work during a telehealth visit with a healthcare provider. Likewise, internet connections can sometimes become unstable due to inclement weather events such as thunderstorms. According to AARP, two in five adults over age 65 feel that technological devices were not designed with them in mind.
Problematically, when a senior-aged person is unable to keep a telehealth visit because of a technology problem, that person is far more likely to not want to use telehealth again. Then, this unfortunate decision can result in your return to driving or escorting your senior-aged loved one to numerous healthcare providers’ offices. In turn, the negative result can be deciding not to keep those needed medical appointments.
Try teaching your loved ones or doing a practice call ahead of time.
These are just three tips to enhancing how a senior can use telehealth for better health and allow caregivers more peace of mind and time away. What else would you add to the list?
Technology in senior care: Enhancing the lives of caregivers and residents alike
June 14, 2024Age Tech,Senior CareBlog
Although many seniors would prefer to stay in their home, a sudden permanent disability can quickly require 24/7 home-based care that can be too expensive or just unavailable. Fortunately, technological solutions now exist that can enable seniors to continue to live independently or in assisted living residences rather than require relocation to a nursing home.
High tech home living and cleaning devices: An aid for seniors plus their caregivers
From technologically-controlled window shades to robotic vacuum cleaners, technology is enabling daily living activities and chores to be more easily accomplished. According to the US Census Bureau, 40% of adults aged 65 and older have at least one disability, of which 66% have difficulty in walking. Owning high tech home gadgets can simplify (and expedite) daily routines. In this way, the senior living independently or in an assisted living residence can maintain more personal independence than otherwise likely.
Videoconferencing technology and its impact on senior health
The widespread adoption of videoconferencing by seniors occurred largely due to the Covid-19 pandemic. As telehealth services began to replace in-person physician office visits during the height of the Covid-19 pandemic, more senior-aged people began to use videoconferencing apps. Through checking in with their doctors and other caregivers via this technology, many seniors were able to manage illnesses and chronic disorders without an in-person visit to do so. In particular, using a videoconferencing app on a Smartphone or computer has enabled seniors to interact with:
- Primary care providers such as physicians and nurse practitioners;
- Physical therapists and nutritionists;
- Psychologists and mental health counselors;
- Family members and friends
Through using telehealth and/or contacting family members online, preventive action to lessen progression to worsened health outcomes was enabled. For example, seniors who had fallen and sprained a knee or ankle could acquire input as to how to treat that sprain to improve faster healing. Thus, a longer period of time for that healing to occur – or a permanent joint disability resulting from improper self-treatment – could be avoided.
Telemedicine linking doctors to specialists: Why this matters for seniors
Many senior-aged people live with heart disease, diabetes (Type-2), kidney disease, or have experienced a stroke. In order to best treat and manage these types of chronic health disorders, primary care doctors typically refer their patients to specialists. For example, cardiologists are heart specialists who can tailor the treatment of a person’s heart disease to their underlying heart disorder and needs. Technological advances in telemedicine are enabling primary care doctors to link online with specialist physicians such as cardiologists to better coordinate their patients’ care.
Whether you are a senior-aged adult or someone caring for a senior, the Ōmcare Home Health Hub® is a technological device that can enable videoconferencing with personal and professional caregivers and managing daily medications. Thus, it can improve safe living in the home or in an assisted living facility.