Empowering family caregivers and improving medication adherence with connected technology
Exclusive technology from Ōmcare aims to offer an unbroken chain of communication between patients, providers, and family caregivers.
By Lisa Lavin, founder and CEO, Ōmcare
The sandwich generation
The United States population is aging and, in the process, they will require more in the way of long-term care support and services. The senior community will more than triple before 2050, with half of these individuals expected to need long-term care, which will come from either skilled nursing facilities or adult children or family members.[1]
Adults who are part of the sandwich generation—that is, those who have a living parent age 65 or older are pulled in many directions. Thirty-five million Americans provided unpaid care to an adult age 50 or older in 2015. The vast majority (85 percent) were caregivers for a relative, primarily an aging parent.[2]
Caregiving for family members takes many forms. Nearly half of family caregivers travel to care for someone, while an additional 35 percent are sharing a home with the loved one they’re caring for. Some are caring for a spouse or partner, many for a parent — all working to help that person stay at home for as long and as comfortable as possible.[3]
Technology’s integration with health care
Amidst rising costs and changing demographic needs, telemedicine has emerged as a viable solution for doctors, patients, employers, and insurance providers to cut costs and save money.
It’s no surprise then that the utilization of telemedicine is growing. According to Deloitte, physicians conducted about 100 million telemedicine appointments globally in 2014, which generated potential savings of more than $5 billion when compared to the cost of in-person doctor visits. And from 2014 to 2018, the use of non-hospital-based provider-to-patient telehealth grew 1,393%.
Another recent report from FAIR Health showed that the use of telehealth services is growing faster than usage at retail clinics, urgent care centers, and emergency departments. The most recent FAIR Health findings show that overall telehealth claims are expected to increase 624% from 2014 to 2018.[4]
By increasing access to physicians and specialists, telehealth helps ensure patients receive the right care, at the right place, at the right time. Currently, 76 percent of U.S. hospitals connect with patients and consulting practitioners at a distance through the use of video and other technology.[5]
New telehealth and remote monitoring technologies are fundamentally changing the way people interact with the health care delivery system.
Connect caregivers with the right technology
From tracking vital signs with remote monitoring devices to communicating quickly with a nurse through a web portal to receiving on-the-spot care from a doctor via video chat, telehealth aims to make life easier.[6]
An AARP study on technology’s impact on caregiving revealed that 68% of caregivers would routinely use technology to manage critical information about patient health, vitals, and document medications. [7]
The right technology can give health care providers and caregivers a means of communication that is essential to improving patient outcomes. For example, patient monitoring programs that allow virtual check-ins enable patients to extend the duration between doctor's visits or unplanned hospital stays. Meanwhile, a KLAS Research report surveying 25 healthcare organizations found that 38% of healthcare organizations using remote patient monitoring programs for chronic disease management reported reduced admissions, while 17% cited cost reductions.[8]
Technology can facilitate this change by tracking and alerting family and medical caregivers in the event of identified house safety problems-fireplace safety, water safety, walking, etc. It can also mitigate environmental variables at home-noise, lighting, temperature-thereby decreasing the likelihood of trouble and resulting habits in people with dementia.
Technology can also play a direct care role in providing voice assistance to the person with dementia for repetitive questions, while delivering helpful input for both the elderly individual and caregivers from trusted circles— family, friends, neighbors, and other caregivers.[9]
Remote patient monitoring benefits patients and care networks
Remote patient monitoring is a digital health solution that captures and records patient physiologic data outside of a traditional health care environment. As providers increasingly turn to remote patient monitoring technology to improve patient outcomes, limit costs and cut down on using more expensive services, healthcare industry newcomers and legacy players alike are vying for a piece of this growing market.
With data collected over time, care team members can manage and treat chronic conditions in a way that is effective, timely, and realistic to the patient and caregiver’s lifestyles. The data generated through this approach can help facilitate conversations between patients and physicians and facilitate opportunities to intervene quickly to avoid complications. Using technology, a patient managing a chronic condition can connect more frequently with their care team from home, and spend less time going to the doctor’s office.
In addition to providing care teams with better, more actionable information earlier, remote patient monitoring has been praised for engaging patients in their care by providing them access to their personal data so they can better understand the impact of their treatment and advocate for their medical needs.
Older adults with long-term care needs should be able to live independently and age while minimizing stress on family caregivers. Telehealth strategies can support this process by improving access to care and ensuring its quality, while reducing the strain put on caregivers that comes from time constraints and managing logistics, added mental and emotional stress, and financial burdens of providing long-term care to an aging loved one. The right technology can address these issues and allow for loved ones to age gracefully and in their best health.
About Ōmcare
Ōmcare is a health technology company aspiring to extend the reach of the caregiver, increase medication adherence, and to improve treatment outcomes by harnessing the power of remote care. We aim to achieve this through our proprietary interactive technologies - promising right pill, right time, right person. By partnering with pharmacies, payers, providers, and family caregivers, our vision is to help people live healthier, more vibrant, independent lives.
[1] "Aging Cost In America." Modern Health Talk. N. p., 2018. Web.
[2] "The Sandwich Generation | Pew Research Center." 30 Jan. 2013
[3] "Caregiving Guides For Families Providing Care At Home". AARP, 2019, Guide to Providing In-Home Care for a Loved One
[4] "Telehealth Use Increasing Most Among Non Hospital-Based Providers." Healthcare Dive.
[5] Fact Sheet: Telehealth - aha.org. Fact Sheet: Telehealth PDF
[6] Telehealth and Seniors | Updated for 2019 | AgingInPlace.org.
[7] Winifred V. Quinn, A., Ellen O’Brien, C. and Greg Springan, M. (2019). Using Telehealth to Improve Home-Based Care for Older Adults and Family Caregivers
[8] "Hospitals Are Finding ROI In Remote Patient Monitoring Programs." mHealthIntelligence. N. p., 2018.
[9] "Telehealth Can Give Caregivers Much-Needed Support, Peace Of Mind." mHealthIntelligence. N. p., 2018.
Image: "Telemedicine & Telehealth Services Covered By Medicare | Medicarefaq." MedicareFAQ. N. p., 2019.
Five new health and caregiving technologies November 2019
LeadingAge in San Diego and more. Entrepreneurs clearly see the opportunity for providing tech-enabled services to help care for older adults. Large events like Leading Age, Argentum, and sub-events within CES and HIMSS all point to the business potential that draws startups as well as new offerings from existing players – in what may become an increasingly crowded market. Here five recent announcements, two from the Startup Garage at Leading Age in San Diego -- adding three others from recent press releases. All information is drawn from the websites of the companies themselves.
Ōmcare (LeadingAge) "Ōmcare is far more than a pill sorting system with self-reported validation. With three issued patents and more pending, Ōmcare’s in-home remote dispensing and integrated care monitoring will drive a new way to measure adherence and set a new standard for care coordination that is simple, safe and easy to use. Ōmcare links remote dispensing with video confirmation such that every dispensing event is directly observed and confirmed. Caregivers know immediately if a dose is missed or incorrectly administered. Other smart pill dispensers and mobile compliance apps depend on self-reporting rather than direct observation. Ōmcare’s approach will change how the industry measures medication adherence." Learn more at Ōmcare.
Read the full article from Aging In Place Technology Watch here.
A test of pills: Ecumen, Thrifty White to join unique telemedicine pilot project
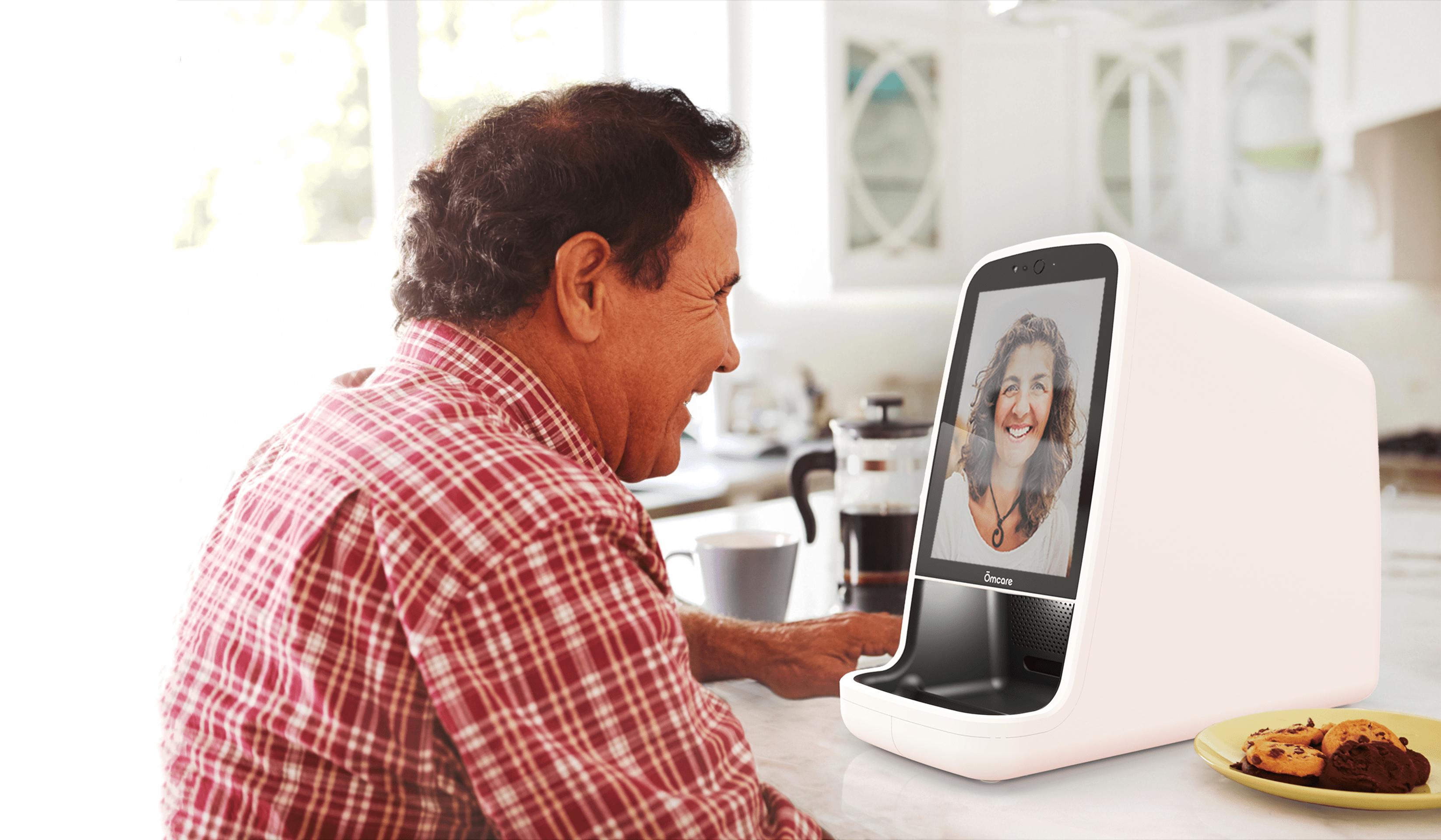
What could be handier? A new machine will dispense prepackaged prescription meds at home, while at the same time allowing the elderly patient to video chat with family and medical staff.
A Burnsville company is partnering with Ecumen and Thrifty White Drug on a pilot project to do just that. Ōmcare has designed its Telemed System to help make sure older adults are taking their medications as prescribed -- at the right time, in the right way.
The Telemed device can hold 15 to 30 days worth of medication, which for the pilot project will be provided by Thrifty White Drug -- individually packaged and pre-slit for easy opening.
The three-way video system allows family or medical staff to call when it’s medication time, and to check in, chat a bit, and make sure the patient is taking the medicine as prescribed.
“It’s the first of its kind, it’s really innovative,” said Brett Anderson, Ecumen vice president of health and clinical services.
Read the full article from the Detroit Lakes Tribune here.
Ōmcare to preview new Telemed System at Leading Age Expo

The secure, interactive Ōmcare Telemed System gives caregivers of all types – from physicians, pharmacists, and home care providers or family members – the ability to see and speak to elderly or disabled dependents and to visually confirm compliance with medication treatment plans from anywhere. Once pre-loaded with pouched, multi-dose medications based on an individual patient’s prescription schedule, the Ōmcare system dispenses medications as scheduled and facilitates remote visual confirmation of a patient’s actions. In essence, Ōmcare is a conduit for telehealth and virtual care services and ultimately provides family members greater peace of mind.
According to Lisa Lavin, the two-way video capabilities of the Ōmcare system can be used by individual caregivers or senior living facilities to ensure proper medication adherence which can significantly impact quality of life and clinical outcomes.
“Sticking to a medication plan can be difficult if our health and mental capacity is compromised. This aspect of caregiving is not only stressful, but it can have significant negative side effects if not done properly,” said Lisa Lavin, founder and CEO of Ōmcare. “The Ōmcare Telemed System fosters care from anywhere and creates a connection between patients, family caregivers, and medical care teams and promises visual confirmation of medication adherence. This level of care and collaboration has been shown to improve outcomes and reduce costs for patients, while creating a more positive experience for all.”
According to Lavin, the company will begin piloting the Ōmcare Telemed System with pharmacy and assisted living partners starting in first quarter 2020 and anticipates direct-to-consumer sales to begin next year, as well.
###
For more information:
Barbara Tabor, APR / (651) 230-9192 / barbara@taborpr.com
About Ōmcare
Ōmcare is a health technology company focused on extending the reach of caregivers, increasing medication adherence, and improving treatment outcomes by harnessing the power of remote care and two-way video technology. By partnering with pharmacies, payers, providers, and family caregivers, Ōmcare strives to help people live healthier, more vibrant, independent lives. Learn more at www.omcare.com. Follow on Twitter (@Omcare_Health) and on LinkedIn.
Connected care and remote patient monitoring prove to be cost-effective methods to improve patient outcomes, medication adherence, and patient satisfaction
Exclusive technology from Ōmcare aims to eliminate common breakdown in chain of communication between patients, providers, and family caregivers.
By Lisa Lavin, founder and CEO, Ōmcare
The United States population is aging and, in the process, they will require more in the way of long-term care support and services. In fact, it’s estimated that between 2015 and 2050, the senior population will more than triple, with half of these individuals expected to need long-term care, which will come from either skilled nursing facilities or from adult children or family members. According to projections produced by the Congressional Budget Office, due to population growth, long-term care expenses could more than double from 1.3% of gross domestic product (GDP) in 2010 to 3% of GDP in 2050.[i]
In either scenario, the high cost of care creates financial hardships for individuals and families, taxes the personal time and relationships between family members, and can even impact the professional lives of caregivers. According to a 2016 report by AARP, family caregivers are spending roughly $7,000 per year ($6,954) in all out-of-pocket costs related to caregiving: household expenses, medical expenses, and more.[ii] The average family caregiver spends roughly $7,000 per year, or nearly 20 percent of their annual income, on out-of-pocket costs, according to AARP estimates.[i]
A common issue that often complicates caregiving, influences patient outcomes, and contributes to rising costs, is lack of medication adherence by patients. Nonadherence accounts for up to 50% of treatment failures, around 125,000 deaths, and up to 25% of hospitalizations each year in the United States.[iii] Studies show that 26% of readmissions are potentially preventable and medication-related, the most common of which was nonadherence due to patient choice (23.8%).[iv]
According to estimates by the IMS Institute, better medication management could produce $213 billion in savings annually, of which $105 billion would be from improved adherence.[v]
The ripple effect of caregiving needs
While the impact of increased caregiving needs for the aging population are many, two of the most significant areas of impact are related to cost and caregivers.
Financial impact. With healthcare costs set to hit more than $2.3 trillion, the need for more cost-efficient care has never been more important. Consider the fact that the annual median cost for nursing facilities ($97,455 for a private room) is more than double the median income of older households ($42,113). Likewise, according to the National Association of Home Care, the average cost of care from a skilled nursing facility is $544 dollars per day, while the average cost of home health care per visit is $132 dollars.[i]
On average, an American turning 65 today will incur $138,000 in future long-term care costs.[ii] Families will pay about half of the costs themselves out-of-pocket, with the rest covered by public programs and private insurance.[x] While most people with long-term care needs will spend relatively little on their care, about one in six (17%) will spend at least $100,000 out-of-pocket.[i]
Caregiver impact. Approximately 35 million Americans provided unpaid care to an adult age 50 or older in 2015. The vast majority (85%) were caregivers for a relative, primarily an aging parent.[vi] The term ‘sandwich generation' – the label used to describe adult children who are simultaneously caring for their children and their aging parents – is becoming so commonplace that it was added to the Merriam-Webster Dictionary in 2006. However, the dictionary fails to mention the heavy financial and emotional stress that being a part of this generation can cause on caregivers.[vi] Caregivers often experience the following:
- Caregivers report high rates of depressive symptoms and mental health problems, compounded with the physical strain of caring for someone who cannot perform activities of daily living, such as bathing, grooming and other personal care activities.[vii]
- 6 out of 10 (61%) caregivers experience at least one change in their employment due to caregiving such as cutting back work hours, taking a leave of absence, receiving a warning about performance/attendance, among others.[viii]
- 49% arrive to their place of work late/leave early/take time off, 15% take a leave of absence, 14% reduce their hours/take a demotion, 7% receive a warning about performance/attendance, 5% turn down a promotion, 4% choose early retirement, 3% lose job benefits, and 6% give up working entirely.[viii]
Further exacerbating these factors is the poor or inconsistent communication that occurs between patients, caregivers, and healthcare providers. A study by the Accreditation Council for Graduate Medical Education (ACGME) found that 69% of health care providers do not have a standardized hand-off process – a real-time process of passing patient information from one caregiver to another – and only 20% have some standardization. This lack of process can create inaccuracies that lead to extended stays in clinical facilities or that complicate medication and therapy adherence outcomes.[ix]
Telehealth solutions impact all stages of care
Amidst rising costs and changing demographic needs, telemedicine has emerged as a viable solution for doctors, patients, employers, and insurance providers to cut costs and save money.[x] It’s no surprise then that utilization of telemedicine is growing. According to Deloitte, physicians conducted about 100 million telemedicine appointments globally in 2014, which generated potential savings of more than $5 billion when compared to the cost of in-person doctor visits.[x] From 2014 to 2018, the use of non-hospital-based provider-to-patient telehealth grew 1,393%.[xi]
New telehealth and remote monitoring technologies are fundamentally changing the way people interact with health care.[xii]
Remote patient monitoring
Remote patient monitoring is a digital health solution that captures and records patient physiologic data outside of a traditional health care environment.[xii] As providers increasingly turn to remote patient monitoring technology to improve patient outcomes, limit costs, and cut down on using more expensive services, healthcare industry newcomers and legacy players alike are vying for a piece of this growing market.[xiii]
Remote patient monitoring is particularly helpful in managing chronic conditions and improving medication adherence because it provides visibility into patients’ lives outside of their scheduled appointments, which has historically been a barrier to timely and effective diagnosis and management.[xiii]
With data collected over time, care team members can manage and treat chronic conditions in a way that is effective, timely, and realistic to the patient and caregiver’s lifestyles. The data generated through this approach can help facilitate conversations between patients and physicians and facilitate opportunities to intervene quickly to avoid complications.[xiii]
In addition to providing care teams with better, more actionable information earlier, remote patient monitoring has been praised for engaging patients in their own care by providing them access to their own data so they can better understand the impact of their treatment and advocate for their medical needs.[xiv]
Connect caregivers with the right technology
From tracking vital signs with remote monitoring devices to communicating quickly with a nurse through a web portal to receiving on-the-spot care from a doctor via video chat, telehealth aims to make life easier.[xiv]
The right technology can give health care providers and caregivers a means of communication that is essential to improving patient outcomes. For example, patient monitoring programs that allow virtual check-ins enable patients to extend the duration between doctor's visits or unplanned hospital stays. Meanwhile, a KLAS Research report surveying 25 healthcare organizations found 38% of healthcare organizations using remote patient monitoring programs for chronic disease management reported reduced admissions, while 17% cited cost reductions.[xiii]
Older adults with long-term care needs should be able to live independently as they age while limiting stress on family caregivers. Telehealth strategies can support this process by improving access to care and ensuring its quality, while reducing the strain put on family members by increased time requirements, added mental and emotional stress, and financial burdens of providing long-term care to an aging loved one. The right technology can address these issues and allow for loved ones to age gracefully and in their best health.
About Ōmcare
Ōmcare is a health technology company aspiring to extend the reach of the caregiver, increase medication adherence, and to improve treatment outcomes by harnessing the power of remote care. We aim to achieve this through our proprietary interactive technologies - promising right pill, right time, right person. By partnering with pharmacies, payers, providers, and family caregivers, our vision is to help people live healthier, more vibrant, independent lives.
References
[i] "Long-Term Services And Supports For Older Americans: Risks And Financing Research Brief". ASPE, 2019, https://aspe.hhs.gov/basic-report/long-term-services-and-supports-older-americans-risks-and-financing-research-brief.
[ii] "Caregiving Innovation Frontiers". Aarp.Org, 2019, https://www.aarp.org/content/dam/aarp/home-and-family/personal-technology/2017/08/caregiving-innovation-frontiers-2017-aarp.pdf.
[iii] Kim, Jennifer. "Medication Adherence: The Elephant In The Room". Uspharmacist.Com, 2019, https://www.uspharmacist.com/article/medication-adherence-the-elephant-in-the-room.
[iv] "Up To 26% Of Hospital Readmissions Are Preventable And Medication-Based". Drug Topics, 2019, https://www.drugtopics.com/drug-topics/news/26-hospital-readmissions-are-preventable-and-medication-based.
[v] IMS Institute for Healthcare Informatics, “Avoidable Costs in U.S. Healthcare: The $200 Billion Opportunity from Using Medicines More Responsibly,” June 2013
[vi] "The Sandwich Generation | What Is The Sandwich Generation?". Seniorliving.Org, 2019, https://www.seniorliving.org/caregiving/sandwich-generation/.
[vii] "Caregiver Health | Family Caregiver Alliance". Caregiver.Org, 2019, https://www.caregiver.org/caregiver-health.
[viii] "Caregiving In The U.S.". Aarp.Org, 2019, https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf.
[ix] Wagner R, et al. CLER 2016 National Report of Findings, Issue Brief #5: Care Transitions. Chicago, Illinois: Accreditation Council for Graduate Medical Education, March 2017.
[x] "Telemedicine Research Papers: Trends In Healthcare - Evisit". Evisit, 2019, https://evisit.com/resources/telemedicine-trends/.
[xi] fairhealth.org. (2019). A Multilayered Analysis of Telehealth. [online] Available at: https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/A%20Multilayered%20Analysis%20of%20Telehealth%20-%20A%20FAIR%20Health%20White%20Paper.pdf.
[xii] "Digital Health Implementation Playbook". Ama-Assn.Org, 2019, https://www.ama-assn.org/system/files/2018-12/digital-health-implementation-playbook-REV1.pdf
[xiii] "The Technology, Devices, And Benefits Of The Growing Remote Patient Monitoring Market". Business Insider, 2019, https://www.businessinsider.com/remote-patient-monitoring-industry-explained.
[xiv] "Telehealth And Seniors | Updated For 2019 | Aginginplace.Org". Aginginplace.Org, 2019, https://www.aginginplace.org/telehealth-and-seniors/.
Ōmcare secures 3rd patent for remote audiovisual medication dispenser
BURNSVILLE, MN (July 31, 2019) — Ōmcare, LLC announced today that the United States Patent and Trademark Office has issued Ōmcare’s third patent (U.S. Patent No. 10,347,377) for the company’s web-enabled, audiovisual, medication-dispensing telemedicine system for the home.
The Ōmcare Telemed System gives caregivers of all types – from physicians, pharmacists, and home care providers or family members – the ability to see and speak to elderly or disabled dependents and to confirm compliance with medication treatment plans from anywhere. The easy-to-use Ōmcare system is designed to facilitate remote monitoring via visual confirmation of a patient’s actions, which supports telehealth and virtual care services and gives family members greater peace of mind.
The addition of this patent will allow Ōmcare to bring products to market that meet the growing demand for remote monitoring technology that supports the long-term goals of improving patient outcomes, medication adherence, and quality of life.
“Our mission is to give caregivers of all types – from physicians, pharmacists, home care providers, and families – the ability to see, speak to, and confirm that patients and loved ones are following their care plans,” said Lisa Lavin, founder and CEO of Ōmcare. “Ōmcare extends the reach of caregivers into the home and promises real medication adherence.”
Lavin, a serial entrepreneur and technology innovator, created Ōmcare after realizing the potential for marrying advances in two-way, remote communications technology with the growing need and consumer demand for in-home care and aging in place. This is the fourth patent for Lavin, who holds three related patents for audiovisual and dispensary capabilities.
###
For more information: Barbara Tabor, APR / (651) 230-9192 / barbara@taborpr.com
About Ōmcare Ōmcare is a health technology company focused on extending the reach of caregivers, increasing medication adherence, and improving treatment outcomes by harnessing the power of remote care and two-way video technology. By partnering with pharmacies, payers, providers, and family caregivers, Ōmcare strives to help people live healthier, more vibrant, independent lives. Learn more at www.omcare.com. Follow on Twitter (@Omcare_Health) and on LinkedIn.
Top 3 reasons connected care requires telehealth
Interest in telehealth is increasing rapidly around the world, including here in the U.S. In fact, the telehealth market has grown over 250% since 2015 and is expected to exceed 15% CAGR* through 2025. This growth is attributed tech-enabled services and a regulatory environment that has started to embrace virtual connected care options.
The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. And while many consumers are just now becoming familiar with the term, it is most often understood as two-way video interactions with doctors or other medical professionals.
#1 - Telehealth is a conduit to enabling value based care
Telehealth has traditionally been considered by CMS as a stop-gap for people with access issues, either in rural area or constrained by limited mobility. A number of progressive health systems that are leading the shift to value based or outcomes based payment see telehealth as a critical component to keeping people healthy, especially seniors with multiple conditions who tend to be heavy utilizers.
#2 - The shortage of caregivers will strain an already strained system.
And for those in the Home Health business, incorporating more frequent remote touchpoints using video-enabled technology along with in-home visits aligns with a desire to create a tighter community of caregivers while offering a response to the new and growing shortage of qualified caregivers. By 2050, there will be 19 million Americans over the age of 85. At the same time, the number of available caregivers is projected to stay constant or decrease.
#3 - Cost avoidance and increased patient satisfaction is more possible.
Ultimately, weaving telehealth into the tapestry of the full healthcare continuum addresses everything from cost avoidance to better outcomes and greater patient satisfaction. And the data proves it. Organizations that embrace technology as a way to define patient needs and deliver personalized care will weather payment system transitions and demographic shifts much more successfully that those unwilling to see the shortcomings of the status quo.
At Ōmcare, we’re building the tele of telehealth right into our core of what we do. From connecting people to integrating a myriad of point solutions and remote monitoring technologies, we can help realize healthier, more affordable outcomes more quickly. Now, that’s healthy. In more ways than one.
What is medication non-adherence? Health and financial risks
Medication non-adherence. It’s a big problem. People are not taking the right pill at the right time. The health and financial risks associated with medication non-adherence impacts individuals, families and caregivers. Today, millions of people depend on others for their medications and, for those who manage multiple medications, it can be complicated and confusing. For many people, loved ones can’t always be there to keep track.
The Financial and Health Risks
Nearly 37% of seniors take 5 or more medications and one out of every ten seniors hospitalized are the result of the consumption of ill-timed, mistaken, or missed medication. The cost of medication non-adherence exceeds $300B and more than 125,000* deaths annually in the United States. That’s a high price to pay for both individuals and the healthcare system more broadly.
In addition to all of this information, it’s important to call attention to the cost of non-adherence at a more personal level, as oftentimes the expense of not taking medications shows up indirectly. The National Council Medical Director Institute published a report in September, 2018 stating that “medication non-adherence accounts for 30-50 percent of treatment failures and 10-25 percent of all hospital and nursing home admissions.” A host of other expenses from the ambulance to the Emergency Room are triggered by non-adherence. These unplanned expenses can be devastating for individuals living on a fixed income, and put additional financial pressure on Medicare and other public programs.
As it relates to better health, the cost of ill-planned or timed drug interactions means risking outcomes that could be debilitating to the patient in more ways than one. For many chronic conditions, improved health outcomes are difficult without proper adherence. A Network for Excellent in Health Innovation (NEHI) study showed that non-adherence could be tied back to an increased risk of hospitalization, while also providing evidence that mortality rate for heart disease and diabetes was 12.1 percent for non-adherence patients compared to 6.7 for adherent patients.** This is just one example of the implications of non-adherence reported in a specific population.
Reducing the Risks
So what can we do to reduce these risks? Several options are: increase access to or engaging the services of a paid caregiver, add more frequent communication with your provider to monitor your adherence activity, or find a technology-enabled medication assistance solution that your loved one can manage on their own. Since most people are reluctant to admit their shortcomings in taking their meds, it’s often unclear when non-adherence has become a liability.
Trust in Ōmcare
That’s why Ōmcare was created: to address medication non-adherence and offer remote care solutions through simple, face-to-face interactions and monitored remote pill dispensing that reduces the risk to financial and personal health outcomes. With Ōmcare you have remote, visual confirmation of adherence and a complete medication history that gives caregivers peace of mind, and provides better information for physicians and nurses to treat and diagnose.
Stay up to date with the latest from Omcare and the release of the Telemed System by subscribing to our email.
Sources:
*https://www.nacds.org/news/the-cost-of-medication-non-adherence/
**Network for Excellence in Health Innovation. (2016, September). Better Uses of Medicines for Diabetes Patients. Retrieved from https://www.nehi.net/writable/publication_files/file/better_use_of_medicine_for_patients_wieth_diabetes_nehi_9.8.2016.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934668/
Healthcare innovation startups: most successful companies of the last 10 years
Today, the healthcare startup scene is booming. With 2018 projected to be the biggest year for investing for the healthcare industry, the future appears promising as more and more groundbreaking companies emerge into the field with bold strategies for solving problems.
However, the healthcare startup landscape wouldn’t be so prosperous without the prominent startups that emerged from the earlier days and succeeded. As the list of startups continues to grow, here are seven of the most successful healthcare startups of the last 10 years.
AbbVie
Headquartered in North Chicago, this biopharmaceutical company was founded in 2013 by Richard Gonzales. Abbvie, which originated as a spin-off of Abbott Laboratories combines advanced science, expertise, and passion to solve serious health issues, which has had a huge impact on people’s lives all around the world. AbbVie currently has ~29,000 employees in over 175 countries and made $28.2 billion in revenue.
Privia Health
A physician practice management and population health technology company, Privia Health works towards keeping people healthy, preventing disease, and improving care coordination both in and outside of the doctor’s office. The private company incorporates key partnerships with employers, health systems and technology, team based-care, and a unique wellness programs to help them on their mission.
Adaptive Biotechnologies
A pioneer and leader in combining high-throughput sequencing and bioinformatics to profile T-cell and B-cell receptors, Adaptive Biotechnologies definitely belongs on this list due to their influence and work within the healthcare sphere. Their immunosequencing platform drives groundbreaking research in cancer and other immune-mediated diseases, which they hope to use to improve patient care and clinical diagnostics.
WeDoctor
Dubbed the “Amazon of healthcare,” WeDoctor is the one of the world’s leading medical health technology platforms. Based in China and founded in 2010 by Jerry Liao Jieyuan, WeDoctor works towards addressing the problem of China’s underfunded and overstretched hospitals. Currently WeDoctor has more than 150 million registered users in China for their online appointment booking, prescription, and diagnostic services. The privately held company is valued at $5.5 billion.
Moderna Therapeutics
Moderna Therapeutics works towards creating MRNA medicines for a wide range of diseases and conditions. Based in Cambridge, MA, the company uses mRNA medicines which allows them to take advantage of normal biological processes to create a desired therapeutic effect. Because of this, they can treat a broad spectrum of diseases, some of which do not have current therapies. Moderna Therapeutics was valued as high as $5B in 2017 by some analysts.
Reata Pharmaceuticals
Reata Pharmaceuticals is biopharmaceutical company that develops drugs for cancer, inflammation, and neurodegenerative diseases. Reata’s mission is to identify, develop, and commercialize novel therapeutics to address serious and life-threatening diseases with few or no approved therapies by targeting molecular pathways that regulate cellular metabolism and inflammation. Reata’s lead product candidates, bardoxolone methyl and omaveloxolone, are Nrf2 activators, which are a transcription factor for restoring mitochondrial function, reducing oxidative stress, and resolving inflammation.
Vezeeta
Vezeeta.com is the leading digital healthcare booking platform and practice management software in MENA that works towards helping the shift towards automated physician, clinic, and hospital bookings to make healthcare more accessible in the region. With over 200,000 verified reviews, patients are able to search, compare, and book the best doctors for them through Vezeeta.
Ōmcare
Our mission isn’t to capitalize on the booming healthcare market, but to push the industry’s success even further with our technology and forward-thinking philosophy. With the Ōmcare Telemed System, we are looking to tackle the problem of medication non-adherence. Of all prescriptions that are filled, 50% are taken incorrectly by the patient. Furthermore, there are 125,000 deaths each year and over $300 billion lost in healthcare costs annually.
At Ōmcare, we are driven to extend the reach of caregivers while enabling face-to-face care from anywhere. Through our technology and innovation, we are actively working towards decreasing the cost of care and empowering patients of all types. We can do what no one else has done before: deliver real medication adherence. We partner with pharmacies, payers, providers, and family caregivers to help people live a healthy, indiependent, and vibrant life no matter their situation.
To stay up to date on the latest news from us, as well as the release of our Telemed System, subscribe to our email.
E Pill vs Med Minder vs GMS Med-e-lert (+ alternatives & reviews)
Medication non-adherence is a serious problem. In fact, it has been linked to many poor health outcomes, including increased hospitalizations and even death. Medication non-adherence ultimately ends up costing the US healthcare system billions of dollars each year.
If you or a loved one is having trouble remembering to take their medication, or if you’re not sure they are taking them correctly, or at all, there is technology available to combat medication non-adherence. We’re going to breakdown three options for you, as well as an alternative to consider.
E-Pill Medsmart Automatic Pill Dispenser

The dispenser is AC powered with a battery backup, and an alarm will sound when the battery is low. When it’s time to take a pill, the E-Pill Medsmart Automatic Pill Dispenser is easy to use, can hold up to 20 aspirin-sized pills at a time per compartment, and can be purchased upfront, with no monthly fees.
“My mom is 89 years old and has a lot of trouble remembering when to take her pills. With the MedSmart pill dispenser that problem has gone away. If the red light is on and the alarm is sounding she knows it is time to take her pills, if not there are no pills in the window and she knows it is not time for her pills. The only regret I have is that I didn't buy this earlier.” - via Amazon Reviews
MedMinder - Jon Pill Dispenser

The Jon Pill Dispenser’s defining feature is that it enables interconnection between the user, their family, and the caregiver. The Jon locking pill dispenser can update MedMinder’s central computer about the patient’s dosage activity, which will then be readily available online for caregivers who can also receive immediate email or text message notifications and weekly reports.
MedMinder Review
“Just want to say how awesome the med minder is! My mother has beginning dementia and AFIB, which messes with her mind and takes 74 pills a day. The MedMinder keeps her on a timely schedule which keeps her med levels more consistent. She is doing better health wise and it gives me peace of mind knowing she doing everything right when I don’t get a text or call.” - via MedMinder website
GMS Med-e-lert

GMS Med-e-lert Review
“Med-e-lert solved my mother's medicine taking problem. Before Med-e-lert, she was forgetting to take her medicine at the assigned times and would occasionally become confused and double dose since all pills were available on her old pill box. All problems solved with this product. It was easy to program and has not jammed or malfunctioned since purchasing it weeks ago. The alarm feature successfully nags Mom until she takes her medicine. I highly recommend this product.” via Amazon Reviews.
Alternative Pill Dispensers (Ōmcare Telemed System)

This product, which will be hitting the market soon, offers caregivers the ability to see, speak to, and confirm appropriate medication from anywhere. The easy-to-use Ōmcare Telemed System enables remote care and visual confirmation of right pill, right time, right person. We want your loved one to feel empowered, not monitored - giving you peace of mind, as if you were right there with them.
Features include:
- 3-way calling capabilities
- Easy, one-touch call interface for end-users
- Medication dispensing, consumption assistance and support
- Remote in-home telehealth care
- Longitudinal data with medication adherence confirmation
- EHR integration to support physician directives
- Ability to dispense multi-dose pouch packaged medication
If you’re interested in making your or a loved one’s life easier by avoiding medication non-adherence, then make sure you keep an eye out for the Omcare Telemed System. Subscribe to our email list to stay up to date on latest updates on the release of this new device!